Monday, November 4, 2002 - 2:48 PM
259
A Validated Objective Measure for Grading the Primary Unilateral Cleft Lip Nasal Deformity
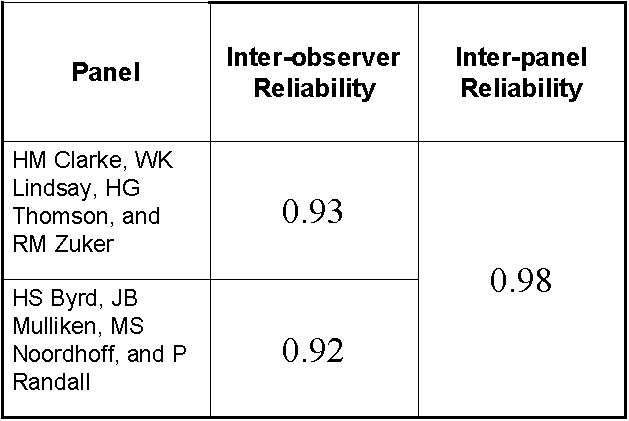
Purpose: The ultimate appearance of the cleft lip nose is influenced heavily by the severity of the primary deformity. Therefore, an outcome is only meaningful in the context of the documented presurgical state. Given a series of patients, it is possible to comparatively express severity of the primary unilateral cleft lip nasal deformity (UCLND) subjectively through ranking. For an individual patient, as is the case in clinical practice, subjective assessment is more difficult due to the absence of direct comparison. The purpose of this study is to develop and provide validation of an objective and quantitative method for gradation of the presurgical UCLND. Our hypotheses are: expert cleft surgeons are able to reliably rank patients according to their subjective assessment of nasal deformity severity and that that one or more objective measurements correlate consistently with this subjective assessment. Materials and Methods: Prospectively, forty consecutive infants undergoing unilateral cheiloplasty were analyzed under anesthesia just prior to surgery. Standardized presurgical photographs and a series of prospectively determined anthropomorphic measurements were obtained. Presurgical photographs were subjectively ranked by four senior cleft surgeons within the institution; internal agreement was assessed. Correlation between measured parameters and subjective ranking was determined. Images were also ranked by four external expert cleft surgeons of international reputation to test the reproducibility of subjective ranking and to validate our measure. Results: Reproducibility was demonstrated by the extremely high correlation (TABLE) of observations among the participants within and between the two expert panels. Of the prospectively measured parameters, the columellar angle was strongly correlated (r=0.73, p<0.0001) and was predictive of the subjective panelís grading. This result was validated by interclass correlation with the ranking of the external expert panel (r=0.79, p<0.0001). Conclusions: Because it is difficult to simplify the complex visual impact of the UCLND, assessment has most commonly been carried out subjectively or categorically (ie. incomplete vs complete). Categorical assignment cannot discriminate significant variation within groups, and subjective assessment is meaningful yet non-quantitative. As we have demonstrated, experts are able to subjectively rank patients with remarkable consistency according to the degree of severity. The columellar angle is an objective and quantitative measurement that varies in a linear fashion with the perceived deformity. It therefore may be useful as an independent and objective indicator of presurgical UCLND severity.
See more of Cranio/Maxillofacial (Including Facial Fractures, Cleft-Lip and Palate)
Back to 2002 Complete Scientific Program
Back to 2002 Meeting home
