Tuesday, November 5, 2002 - 3:26 PM
902
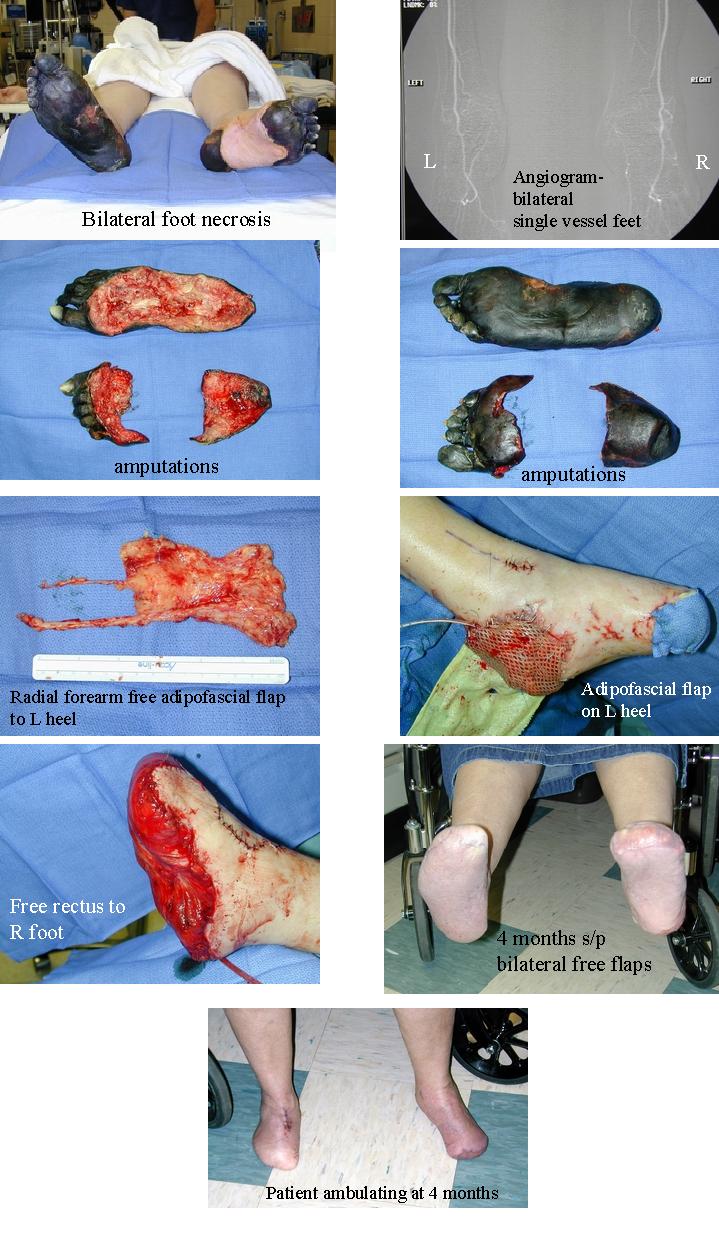
Limb Salvage of Lower Extremity Wounds with Free Tissue Transfer in Difficult Patients
Microvascular free tissue transfer has revolutionized the treatment of lower-extremity wounds. However, amputation is still frequently recommended to patients with complex lower-extremity wounds and/or significant medical conditions because limb salvage after free tissue transfer in these patients remains uncertain. In the past 3 years, more than 75 free tissue transfers to lower extremities were performed at our institution. Among them, eighteen patients (13 males, 5 females, age 17-71 years) with complex wounds in their lower-extremities and/or significant medical conditions had free tissue transfers for limb salvage. Seven patients had extensive soft tissue defect (>1/2 length) of the legs or feet and 6 had composite tissue defect of the legs or feet requiring bony reconstruction. Two patients had both bony and extensive soft tissue defects. An additional 5 patients also had significant peripheral vascular problems due to various medical conditions. A total of nineteen free tissue transfers (16 free muscle flaps, 2 osteomyocutaneous flaps, and 1 adipofascial flap) were performed in 18 patients (One patient had bilateral transfers, see figures below). A saphenous vein loop or graft was used in 3 patients. Free tissue transfer was successful in 16 of 18 patients (89%). Flap loss occurred in 2 patients (One at 2-week post-op) and both were treated successfully with either a second free tissue transfer or pedicle flaps. Four (4/17, 24%) patients required reoperation for salvage of a free flap. A bone graft was done subsequently in 4 patients. Successful limb salvage has been achieved in all 18 patients (18/18, 100%) with a healed wound for up to 30 months. Thus, we believe that free tissue transfer for limb salvage in difficult patients is still a worthwhile procedure and should be attempted if possible. Meticulous pre-op preparation and intra-op execution combined with the use of innovative microsurgical techniques are the keys for success.
View Synopsis (.doc format, 24.0 kb)
See more of Microsurgery
Back to 2002 Complete Scientific Program
Back to 2002 Meeting home
