Wednesday, October 29, 2003
3174
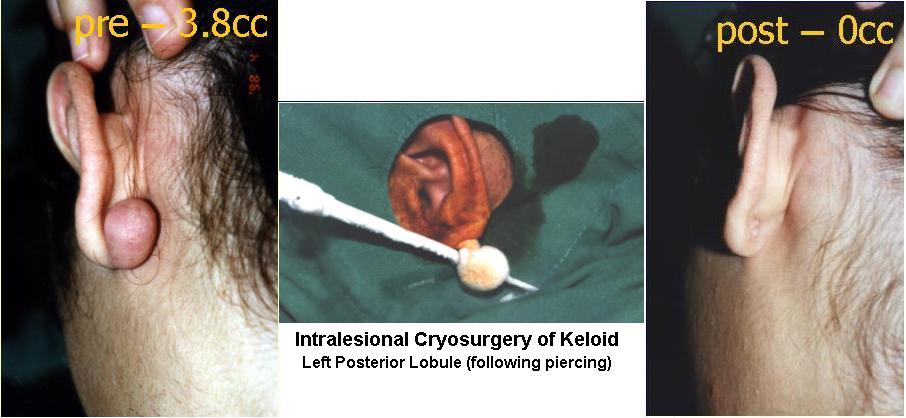
Intralesional Cryotherapy for Enhancing the Involution of Hypertrophic Scars and Keloids
Purpose: Although therapeutic management of hypertrophic scars and Keloids (HSK) using contact or spray cryosurgery was shown to yield significant improvement or complete regression of HSK, it requires 1-20 treatment sessions. This study was designed to assess the clinical safety and efficacy of an intralesional needle cryoprobe method in the treatment of HSK.
Patients & Method: Twenty four caucasian patients (15 males,9 females) ranging in age from 3 to 76 years, with a total of 26 HSK with a volume between 0.65 to 6.0 cc, of more than 6 months duration and of diverse causes were included in this study. The 18-month trial evaluated volume reduction (using impression material and water displacement method) of the HSK following a single session of intralesional cryotherapy. Objective (elevation, hardness and color) and subjective (pain, tenderness and itchiness) parameters were examined on a scale of 0 to 3 (low score was better). The clinical scores and scar volumes before and after treatment were compared using the Wilcoxon test for pairs. Biopsies for Pre- and post-treatment histomorphometric studies of the HSK collagen fibers included spectral Picrosirius red polarization and Fast Fourier Transform orientation index.
Procedure: The novelty of this cryoprobe (U.S.patent number 6,503,246) is its specially designed uninsulated, elongated cryoneedle that has an inbuilt safety cryogen vent and a sharp-cutting tip so to easily penetrate the often hard, rubbery and dense HSK. This cryoneedle is inserted into the long axis of the HSK so as to maximize the volume of the HSK to be frozen. The cryoneedle is connected by an adaptor to a cryogun filled with liquid nitrogen, which is introduced into the cryoprobe thereby freezing the HSK (temperature is lower than -22°C). After the HSK is completely frozen, the cryopneedle defrosts and is withdrawn.
Results: A mean volume of 56.19 % of scar volume reduction was achieved following one session of intralesional cryosurgery treatment (Mean ± STD preoperative HSK volume (cc) = 2.41 ± 1.71; Mean ± STD post-treatment volume= 1.14 ± 1.0; p< 0.01). The time needed to achieve complete freezing was between 5 to 35 minutes. Significant reduction in objective and subjective clinical symptoms was documented, i.e., percent of improvement: elevation- 91.67, hardness-83.33, color- 75.0; pain- 41.67, tenderness-91.67 and itchiness- 75.0. Mild pain or discomfort during and after the procedure was easily managed. Only mild local edema and epidermolysis, followed by a short re-epitheliazation period, were evident. During the 18-month follow-up period there was no evidence of bleeding, infection, adverse effects, recurrence, or permanent depigmentation. The histomorphometric analysis demonstrated rejuvenation of the treated scars, i.e., parallelization, and a more organized architecture of the collagen fibers when compared to the pre-treated scars.
Conclusion: The results of this study demonstrate a significant efficacy of this method due to increased freezing area of deep scar material when compared to that obtained with commercially available contact/spray cryoprobes. As a result, fewer treatment cycles are needed. Since the re-epitheliazation period is decreased, treatment intervals-if any can be shortened to 2-3 weeks. This intralesional cryosurgery method, which is a further promising technical improvement in the obdurate treatment of HSK, is simple to operate, safe to use, necessitates less postoperative care of the wound, and can easily be added to any preexisting cryosurgical unit.
View Synopsis (.doc format, 68.0 kb)
See more of General Reconstruction
Back to Plastic Surgery 2003 Complete Scientific Program
Back to Plastic Surgery 2003 Meeting home
