Sunday, October 10, 2004 - 7:55 AM
5721
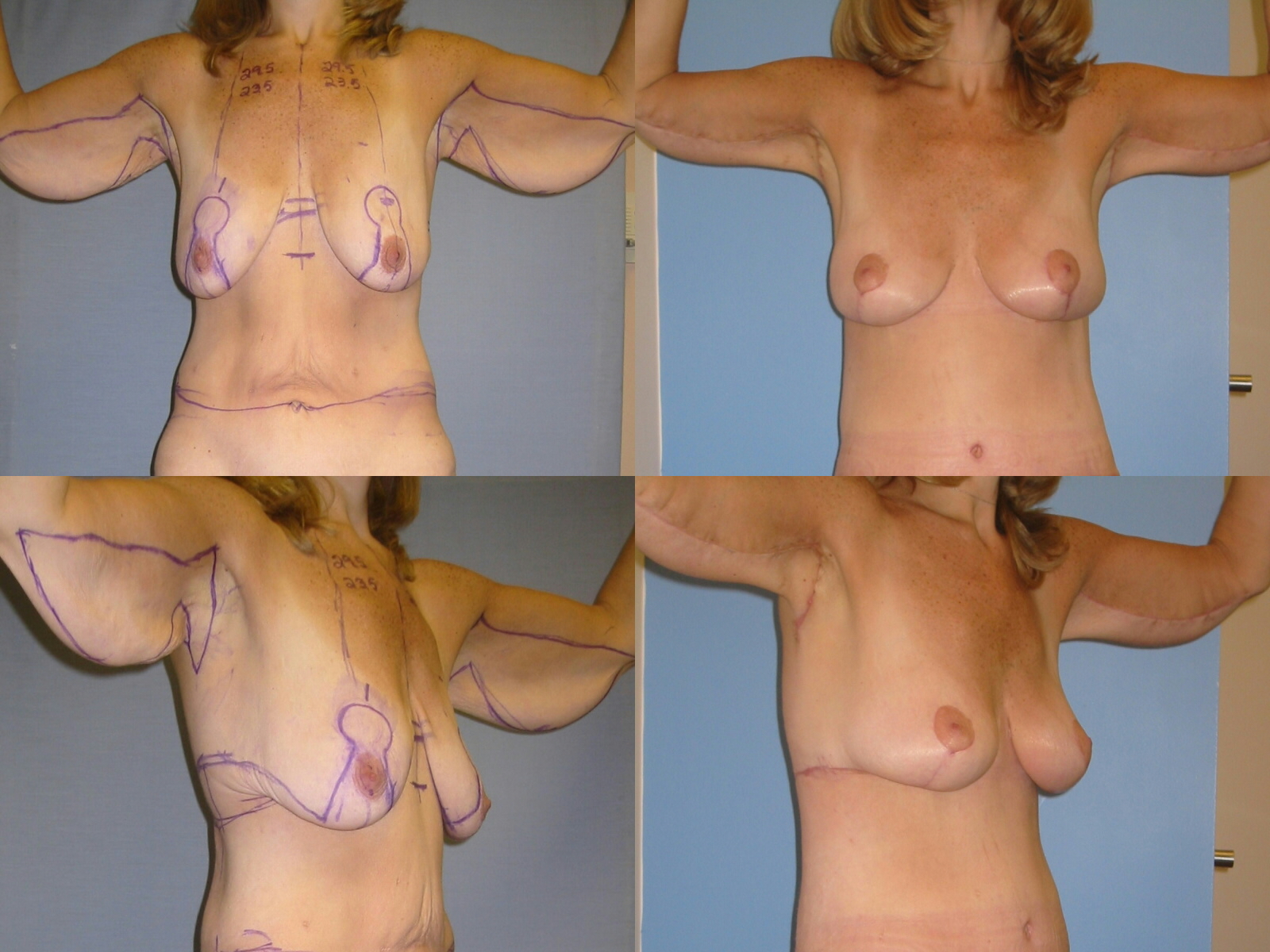
Brachioplasty in the Massive Weight Loss Patient
Introduction: After massive weight loss, most patients suffer from severe hanging skin of the upper arms. This wing-like deformity includes descent of the posterior axillary fold, which flows into a lateral chest and back roll. Previously described techniques do not address this complex problem. We present a new technique that corrects these deformities, leaving one continuous, inconspicuous non contracting scar across the axilla. The results over that past four years at the University of Pittsburgh were reviewed. Materials and Methods: When the extent of the deformity became clear, the excision pattern was changed and extended to the lateral chest. This technique has been applied to 18 of our 72 body contouring patients. See figure of 34 year old woman who lost 180 pounds ans is pre and six weeks after brachioplasty with a Total Body Lift. Excess skin and fat is excised from the inner aspect of the arm from the axilla to the medial epicondyle in the form of a horizontal hemi-ellipse with the superior undulating line along the bicipital groove rising to the deltopectoral groove. The inferior excision line loops along the posterior margin of the hanging skin. The distance between these lines represents the predetermined area of excision. A second hemi-ellipse drops vertically to include the lateral half of the oversized axilla and some redundant lateral chest skin. The two ellipses lie at right angles and overlap at the axillary arm junction. A triangular flap of inner arm skin forms inferior to these vertical and horizontal ellipses. The entire pattern is incised through the crural fascia. Excision proceeds over the cural and clavipectoral fascia and completed over the serratus fascia, taking care to preserve the intercosto-brachial nerve. Liposuction is performed as necessary. The wound edges are approximated with towel clips with advancement of the tip of the inferiorly based triangle to the deltopectoral groove to correct the descended posterior axillary fold. 2-0 PDS closure of the subcutaneous fascia and 3-0 PDS running intradermal closure completes the operation. Elastic sleeves are worn for about three weeks. Results: There were no hematomas, infections or dehiscence’s. Six patients had tip necrosis of the V advancement flap, which healed without secondary procedures. 15 of the 18 patients were pleased with the one stage operation and the scars. Further skin reduction and/or scar reduction were performed in three patients. Conclusion: An effective, reliable and safe brachioplasty technique has been applied to a wide spectrum of deformity in 18 patients after massive weight loss. Integrating the brachioplasty into the upper body lift improves the contour of the upper lateral chest. The zigzag course of the scar across the axilla has inhibited scar contracture with no banding or restriction of arm movement.
View Synopsis (.doc format, 71.0 kb)