McCormick Place, Lakeside Center
Sunday, September 25, 2005
9:00 AM - 5:00 PM
McCormick Place, Lakeside Center
Monday, September 26, 2005
9:00 AM - 5:00 PM
McCormick Place, Lakeside Center
Tuesday, September 27, 2005
9:00 AM - 5:00 PM
McCormick Place, Lakeside Center
Wednesday, September 28, 2005
9:00 AM - 5:00 PM
8120
Ptosis and the Inframammary Fold: Liposuction as an Adjunct for Refinement in Implant Breast Reconstruction
Plastic surgeons have long recognized the importance of creating a well-defined inframammary fold during breast reconstruction. Amidst the available techniques and surgical approaches, defining the inframammary fold remains one of the key elements in successful breast reconstruction. In addition, ptosis of the reconstructed breast is usually required, and the creation of ptosis is an essential component of inframammary fold placement. This paper describes an efficient and effective method to help achieve a more well defined inframammary fold and natural ptotic appearance of the breast.
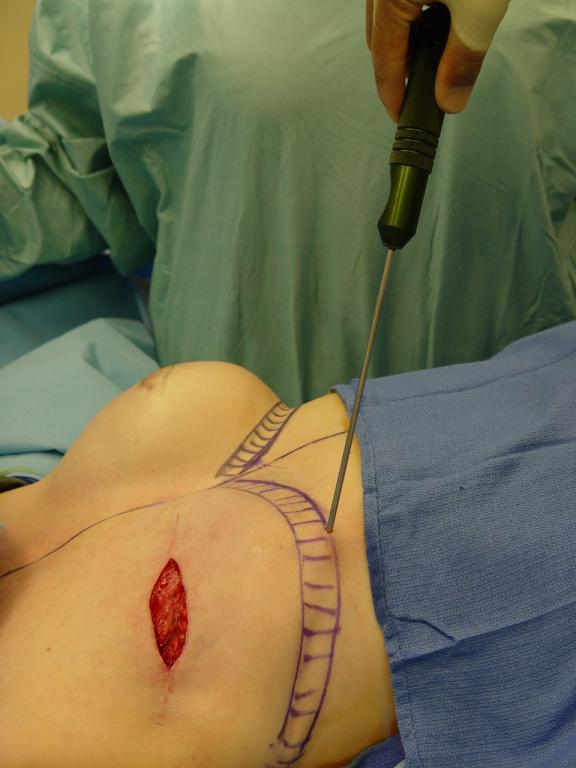
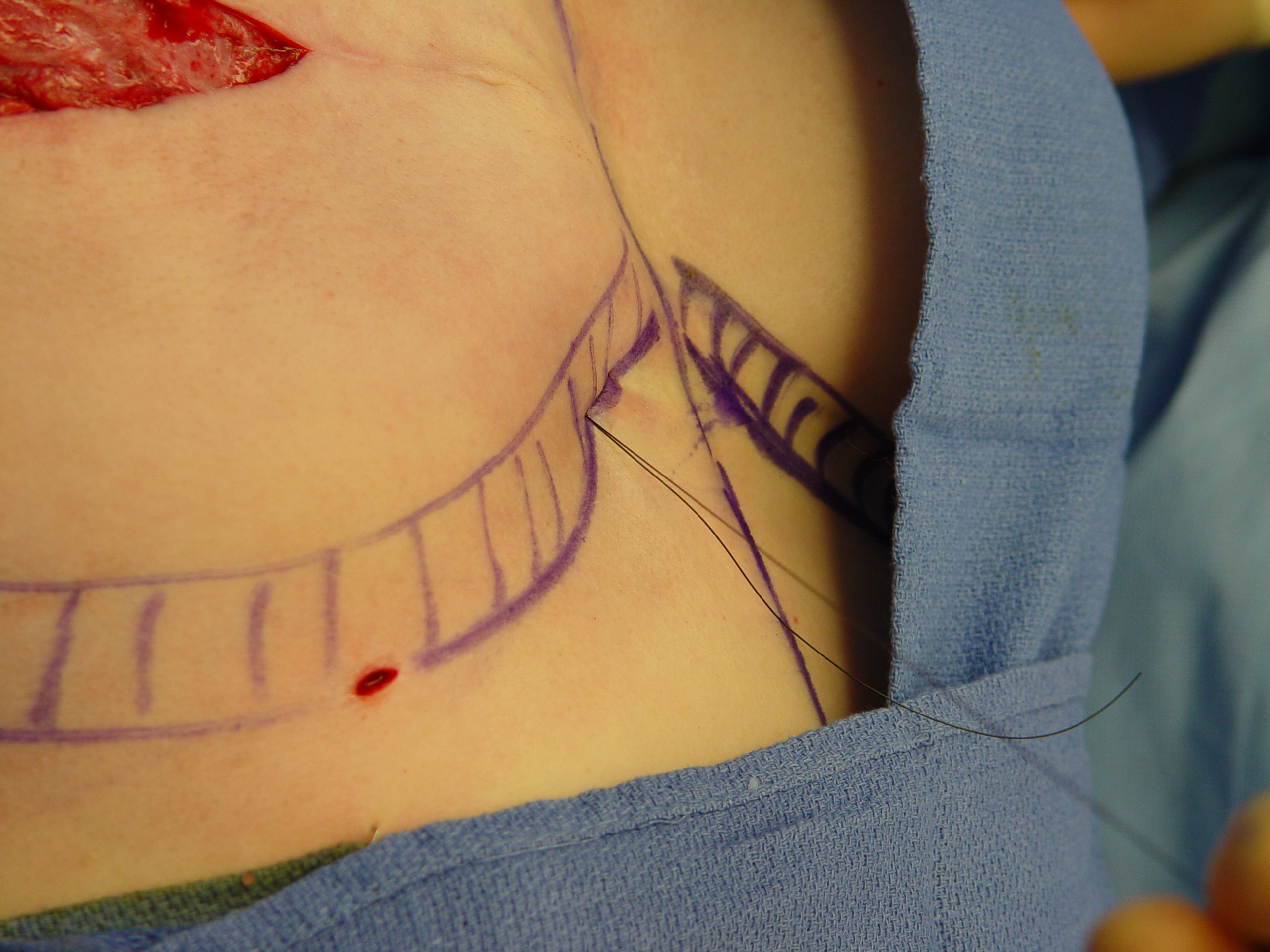
The essential components of this technique are thoracoepigastric skin advancement as described by Ryan and others, combined with liposuction to thin the flap at the level of the proposed inframammary fold. Liposuction is especially critical when operating on the obese patient, or when there is excess subcutaneous fat at the inframammary fold. Previously described epigastric advancement techniques are difficult to apply when the flaps are too thick because of excess subcutaneous fat. Excess flap thickness precludes adequate folding of the advanced skin at the inframammary fold, and sutures at the fold may be under too much tension. Either of these situations may lead to breakdown of the inframammary fold reconstruction, and malposition of the implant. A tight, well-defined crease can be created when liposuction is performed prior to placement of the plication sutures at the inframammary fold. Tissue expanders are placed as Stage 1, followed by Stage 2 expander-implant exchange. The creation of breast ptosis proceeds as described by others, except that the epigastric advancement flap is aggressively thinned with liposuction prior to undermining(Figs. 1,2). Periprosthetic capsular tissue is preserved, and capsulorraphy proceeds as has been described by Dowden and others. Upon completion of liposuction, the epigastric skin is undermined and advanced: more ptosis is achieved with more undermining and advancement. 2-0 nylon horizontal mattress plication sutures are placed to secure and contour the inframammary fold, and each suture incorporates the inferior edge of the posterior capsule(Fig. 3). This defines the location and shape of the inframammary fold(Fig. 4). The outcome from this liposuction refinement demonstrates an improvement in aesthetic results in breast reconstruction (Fig. 5). From January 2003-January 2005, this procedure has been performed on 50 patients. Thirteen of these patients had bilateral reconstructions. In these 63 breasts, there have been 5 complications(7.9%). Only one patient(1.6%) experienced breakdown of the inframammary fold reconstruction, and inferior descent and malposition of the implant resulted. In 2 cases(3.2%), the creation of tight, well-defined inframammary creases caused an unacceptable “high and tight” appearance of the breast reconstructions. This was successfully remedied in both cases by changing to smaller implants at the time of nipple-areola reconstruction. There was 1 case(1.6%) of implant exposure, not at the inframammary fold, but at the lateral aspect of the mastectomy incision where an axillary scar contracture was released. One patient(1.6%) elected to have her saline implants exchanged for silicone gels.
Creation of ptosis and a well-defined inframammary fold takes more time than a simple exchange of tissue expander for permanent implant. Liposuction to thin the skin flap at the inframammary fold, especially in the heavy patient, is a critical addition to the armamentarium of the breast reconstructive surgeon. These adjunctive procedures greatly add to the natural appearance of the breast reconstruction, and can be performed with an acceptable complication/reoperation rate.
Figure 1: Shaded areas demonstrate where liposuction and undermining are planned
Figure 2: Liposuction at the inframammary fold, including skin to be advanced
Figure 3: Horizontal mattress plication sutures placed at the inframammary fold.
Figure 4: Inframammary fold defined. Note degree of ptosis with skin advancement
Figure 5: Final implant after completed refinement procedure on right compared to tissue expander on left prior to refinement procedure. Note that the shaded area on right has been advanced and contributes to breast ptosis
View Synopsis (.doc format, 30.0 kb)