Tuesday, September 27, 2005 - 8:40 AM
8594
Association of Allogenic Bone for Flap Prefabrication: An Experimental Study
Introduction: Extensive bone loss is still a challenge for reconstructive surgery especially in pediatric patients. The use of allogenic bone can be an alternative with no donor area morbidity and unlimited amount of bone. However large bone grafts have problems in revascularization and non-unions. Moreover infections occur more often than with small bone fragments or autografts. Better results can be achieved after bone preparation and adding a vascular supply, which can be done along with flap prefabrication.
Methods: Forty-two Wistar rat bone diaphisis were prepared and distributed in two groups: Group 1: demineralized/liophilized and Group 2: deep freezing (-70 oC). Two bone segments (one of each group) were implanted in rats of the same species in order to prefabricate flaps using superficial epigastric vessels (Figure1). These flaps remained in their respective groin regions until the sacrifice occurred with 2 weeks (n=7), 4 weeks (n=7) and 6 weeks (n=7). Histological sections of undecalcified bone were prepared. A semi-quantitative analysis based on histology (tetracycline marking, cortical resorption, number of giant cells and vascularization) and a quantitative analysis based on histomorphometric parameters (osteoid thickness, cortical thickness, and fibrosis thickness) were performed. Along with histology analysis, TGF-b imunohistochemistry staining was done.
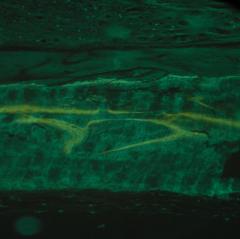
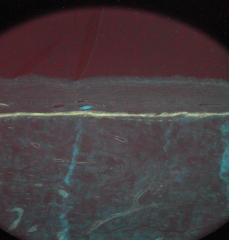
Results: Tissue responses to different bone preparations were distinct: Group 1 fragments presented osteoid matrix on their external surface in all times (Figure2). Some of them had cartilage formation and mineralization areas. These findings were not observed in Group 2 fragments. Group 1 had more mineralization and double tetracycline marks which were almost not seen in Group 2 (Figure 3). Cortical resorption and number of giant cells were greater in Group 2 all times. Vascularization time and fibrosis thickness were very similar in both groups in all times. Concerning the imunohistochemistry, Group 1 had more intense TGF-b staining by two weeks. Nevertheless from 4 weeks on Group 2 presented statistically significant stronger staining.
Conclusions: Both methods for preparing bone produced suitable materials for prefabrication of flaps. Ought to the osteoid matrix formation and higher mineralization rates, Group 1 bone fragments are more osteogenic and should be preferred when the intention is to get an autogenic bone substitute. Nevertheless Group 2 fragments can be more resistant to compression and would be more appropriate to be used in reconstructions that will be submited to higher mechanical stress. Both groups presented good vascularization by two weeks suggesting that the prefabricated flap was ready to be used by that time. TGF-b imunohistochemistry differences occured in Group 1 probably because it was related to bone osteoinduction while in Group 2 it could be related to the inflammatory response alone or along with bone resorption.
Figure 1: Bone prefabrication.
Figure 2: Cortical bone (pink) of Group 1 fragment 4 weeks after flap prefabrication. Osteiod matrix is seen over the cortical bone (sky blue) and has some remineralization areas (40x).
Figure 3: Mineralization evaluation with tetracycline: double marking of Group 1 fragment, 4 weeks after prefabrication (left) and single continuous marking in a bone fragment of Group 2 (right).
View Synopsis (.doc format, 463.0 kb)
See more of Hand, Upper Extremity/Microsurgery
Back to 2005am Complete Scientific Program