McCormick Place, Lakeside Center
Sunday, September 25, 2005
9:00 AM - 5:00 PM
McCormick Place, Lakeside Center
Monday, September 26, 2005
9:00 AM - 5:00 PM
McCormick Place, Lakeside Center
Tuesday, September 27, 2005
9:00 AM - 5:00 PM
McCormick Place, Lakeside Center
Wednesday, September 28, 2005
9:00 AM - 5:00 PM
8607
Three-Dimensional Body Scanner; an Aid in Planning Body Contouring Surgery
THREE-DIMENSIONAL BODY SCANNER: AN AID IN PLANNING BODY CONTOURING SURGERY
PURPOSE:
Modern technology has developed a body scanner that creates an accurate three-dimensional subject image. The purpose of this study was to collect and compare standard body contouring data from scanner and anthropometric measurements, the accepted “gold standard”. Forecasted models of prospective body contouring procedures were then mathematically developed for the purpose of developing 3-D views of multiple predictive outcomes.
METHODS AND MATERIALS:
The scanner used white light phase profilometry to rapidly produce a three-dimensional image of the subjects. The scanner measured suprasternal-notch-to-nipple and nipple-to-nipple linear lengths and bust, contoured-bust, under-bust, waist, hip, abdomen, thigh and knee circumferences. These findings were compared to anthropometric measurements on the same subject population.
EXPERIENCE:
In a 12 month period we scanned and anthropometrically-measured 72 subjects [16 breast augmentations, 7 mastopexies, 26 breast reductions, 20 abdominoplasties, 34 bilateral lipoplasties and 3 gynecomastia reductions]. In addition, 5 breast augmentations, 4 breast reductions and 4 abdominoplasties underwent “predictive modeling” in real time, during surgery, to facilitate accurate post-operative results.
SUMMARY:
The results of this study demonstrated the safety, efficacy and reliability of the white light scanner. Lin's Concordance Coefficient [LCC] indicated that digital scanning was as accurate as and more efficient than anthropometric measuring. For breast augmentation, both pre- and post-operative linear measurements demonstrated pronounced concordance: >0.67 [.67 pre-op to .89 post-op]. Breast circumferential measurements also demonstrated a high LCC between the scanner and anthropometric measurements pre- and post-operatively: >0.79 [0.79 pre-op to 0.89 post-op]. The LCC's became more concordant postoperatively. Similar statements can be made regarding the concordance of the linear measurements taken on breast reduction subjects. Preoperative breast circumference measures were highly concordant for the bust [LCC=0.81], but other circumferential measures were moderately concordant [LCC=0.40-0.57]. Postoperatively, all time intervals demonstrated a strong concordance [LCC>0.67, range: 0.67-0.92] for all circumferential measurements. For abdominoplasty subjects, hip, waist and thigh circumferential measures were concordant across all intervals: >0.54[0.54pre-op to 0.96post-op]. Moreover, the ability to electronically derive the scanner measurements simultaneously suggested that the scanner provided greater efficacy in clinical settings. We also employed the scanner as a predictive tool for body contouring. “Measurement tools” and “embedding tools” within a “Virtual Surgery Suite” allowed the virtual surgeon to volumetrically manipulate the subject's pre-operative contour to correctly shape to the desired shape.
CONCLUSIONS:
The objectives of this study- to measure and compare scanner and anthropometric measurements and to describe predictive modeling - were met and reinforced. Our initial hypothesis, that digital technology was valid and could be applied to accurately record body contouring results, suggested that the scanner provided greater efficacy than anthropometric measurements in clinical settings. The sequential hypothesis, that predictive modeling could be used to advantage by both surgeon and subjects, was demonstrated by accurate real-time forecasted modeling, validation comparisons and data archiving. The figure below displayed the pre-operative patient's scan image in the native 3D data modeling format.
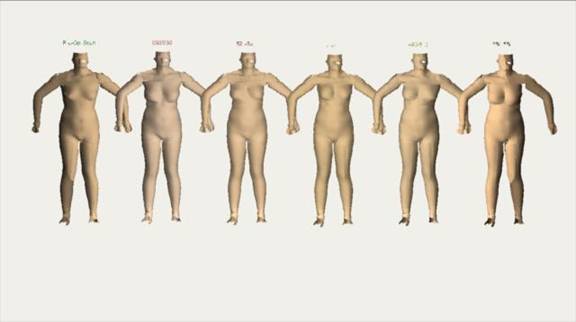
Figure 1. Pre-operative subject's 3D scan image.
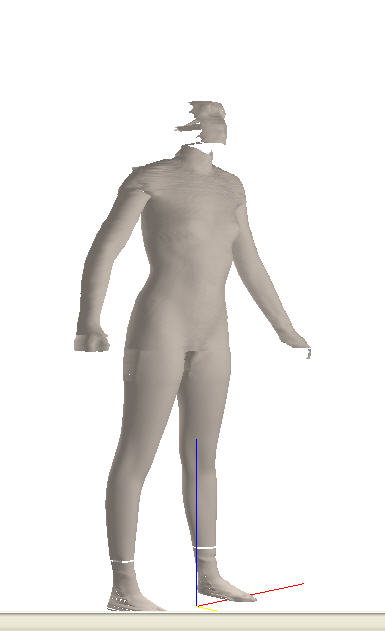
Figure 2. Pre-operative breast augmentation subject's scan image with measurements highlighted.
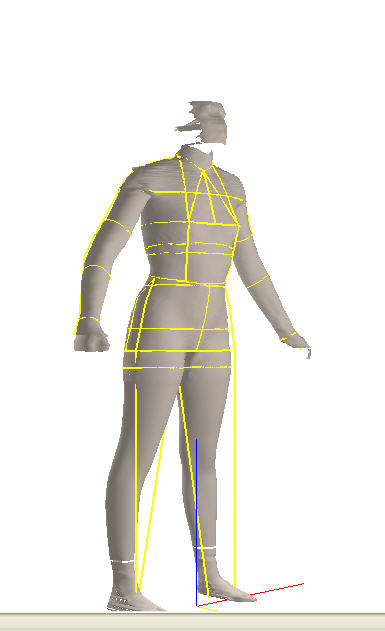
Figure 3. Pre-operative measurements extracted from the subject's 3D scan.
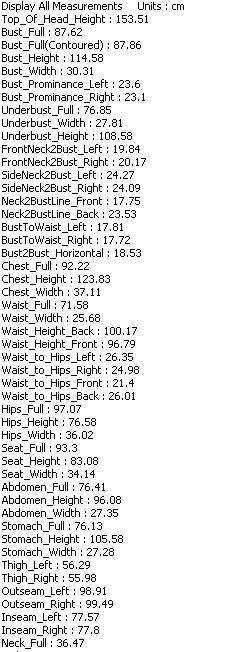
Figure 4. Pre-operative breast augmentation subject translated into an editable polyhedral structure.
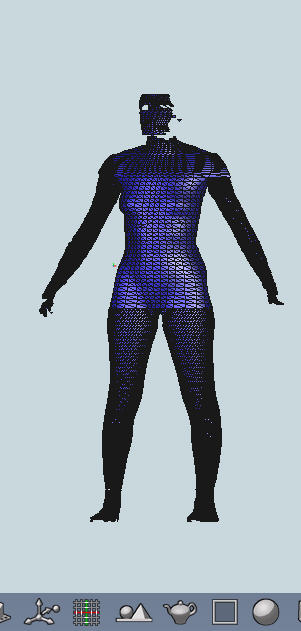
Figure 5. 345 cc Mentor 1600 Smooth Round virtual breast implants.
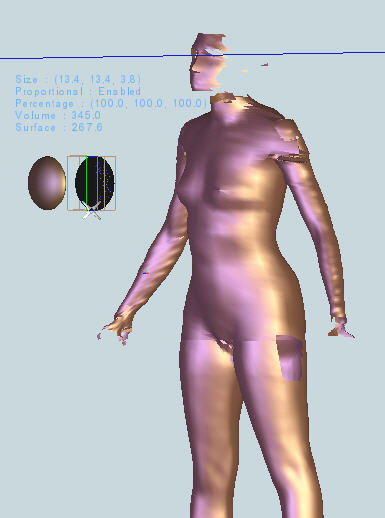
Figure 6. Placement of the virtual implants.
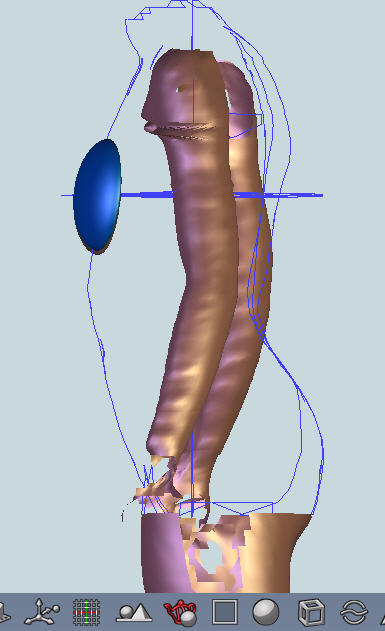
Figure 7. Embedding the virtual implants.
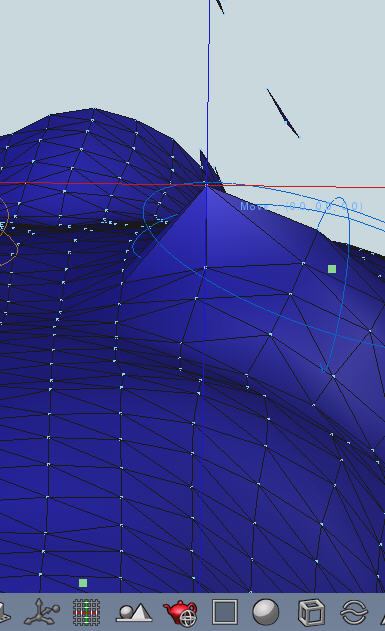
Figure 8. The forecasted 3D model.
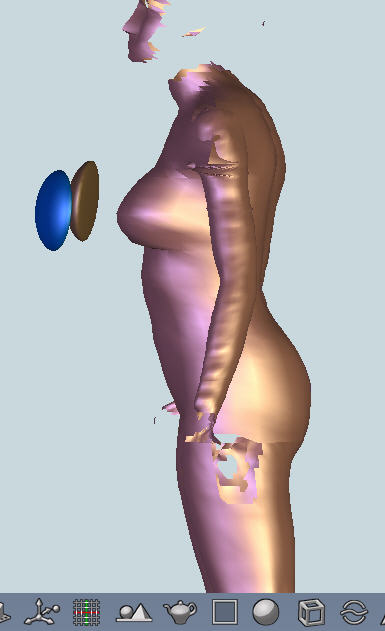
Figure 9. The forecasted 3D model translated back into scanner format.

Figure 10. Measurements extracted by applying from the forecasted model
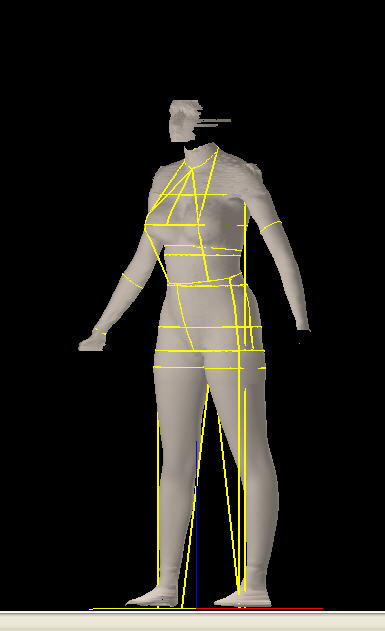
Figure 11. 7 Month Post-operative subject scan.
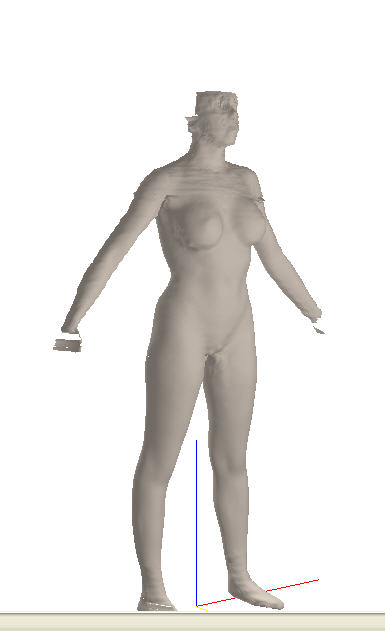
Figure 12. 7 Month Post-operative subject scan measurement extraction.
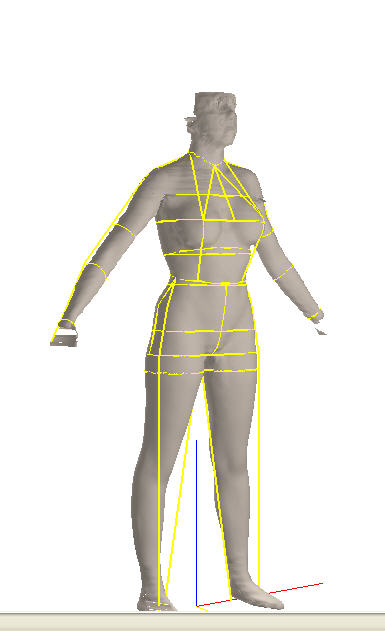
Figure 13. 7 Month Post-operative subject's extracted measurements.
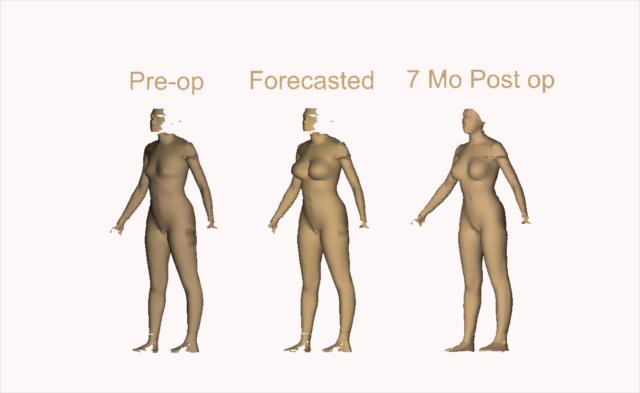
Figure 14. A 3D composite comparison image.
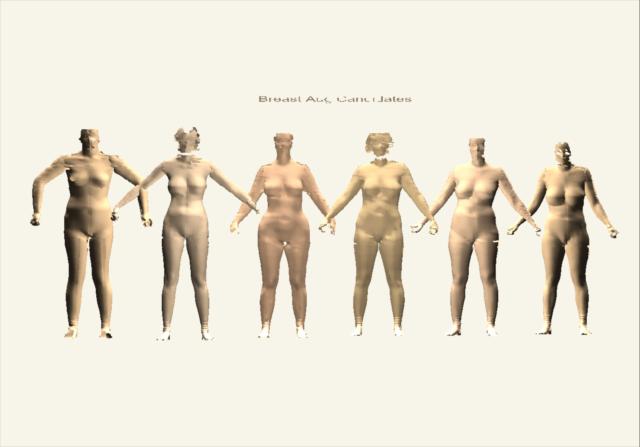
Figure 15. Another 3D composite comparison image – grafting technique.
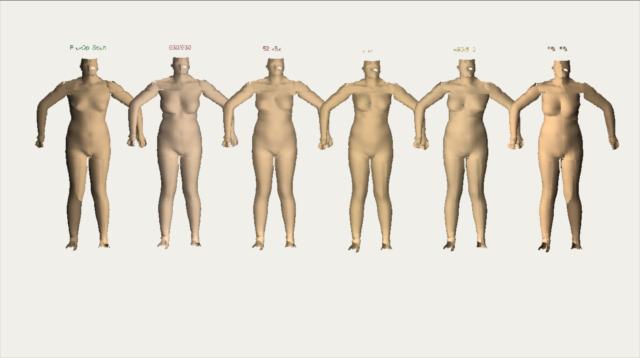
Figure 16. A 3D composite comparison image post-op breasts”grafted” on pre-op subject.