Sunday, October 8, 2006
10309
Reconstruction of Orbital Blowout Fracture Using an Ultrathin Woven Micro Titanium Mesh
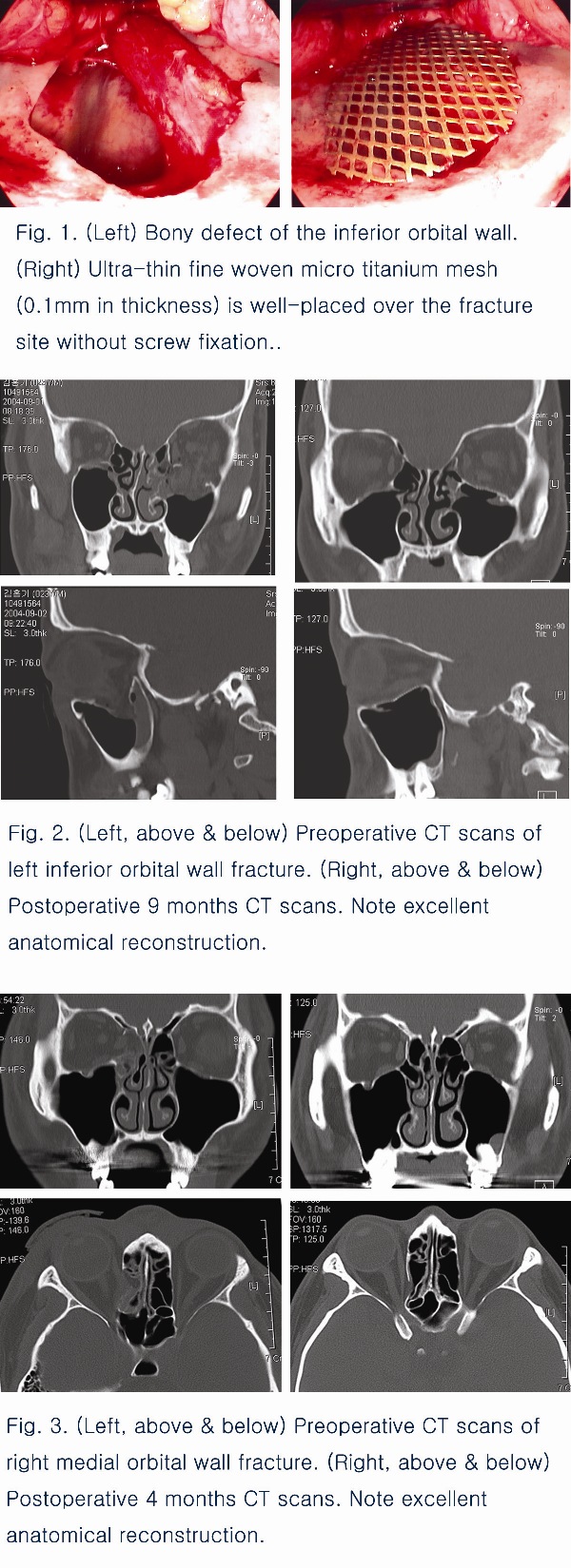
The treatment of orbital blow out fracture consists of orbital content reduction and orbital wall reconstruction, spanning the defect with autogenous or alloplastic materials, and restoring the correct anatomy and volume of the orbit. The optimal material for orbital reconstruction remains controversial. Although various autograft or synthetic materials for orbital wall defects have been used, there is still no ideal reconstruction method. Any material used to span the defect should provide enough structural support and reestablish the pre-injured orbital volume. It should also be biocompatible with the surrounding tissues and easily reshaped to fit the orbital wall. For this purpose, we used the fine woven micro titanium mesh ( 0.1 mm thickness ) for reconstruction of orbital wall fracture. The 169 patients who had medial, inferior or inferomedial orbital wall fractures during three years were included in this study. Reconstruction of the orbital wall was performed following the subciliary approach for inferior side and local approach through W-shape incision on the superior medial orbital area for medial side. After freeing and complete restoration of the entrapped soft tissues, small bony fragments were removed. The titanium mesh was trimmed and moulded depending on the extent and site of the defect. The mesh was then inserted in a subperiosteal plane ensuring that the margins rested on firm bone. No fixation of the mesh was required. Patients were follow up during 3 up to 12 months after surgery. The most patients had a good anatomical reconstruction, but there were 4 cases of enophthalmos, 8 cases of displacement of titanium mesh and 2 cases of maxillary sinusitis. There was no extrusion, hematoma and fibrous capsule. The two patients of severe displacement had re-operated with titanium mesh. As ultra-thin woven micro titanium mesh which consists of many micro pore (49/Cm2) has characteristics such as good drainage of exudates and excellent biocompatibility, it has lower potential of hematoma and infection. Also connective tissue can grow around and into the implant micro pore, preventing its migration. Its thin native allows for easy trimmming and moulding exactly to the orbital contour. As it has good physical strength, this permits the bridging of larger defects than with materials which tends to sags. Therefore ultra-thin woven micro titanium mesh can be safely used in orbital wall reconstruction and can be another reliable treatment alternative.
View Synopsis (.doc format, 240.0 kb)