Wednesday, October 31, 2007 - 8:15 AM
12581
A Randomized, Prospective, Parallel Group Study Comparing an Ultrasonic Scalpel to Electrocautery in Abdominolipectomies
Purpose: Abdominolipectomy is performed to correct abdominal skin and fat redundancy and muscle diastases. Persistent serous wound drainage (extended closed suction drainage) and seromas are the most common complications in abdominolipectomy. Prolonged use of drains can delay healing, cause injury, and increase the risk of retrograde infection and patient discomfort. Furthermore, wound drainage has a direct correlation with seroma formation. The use of the Harmonic ultrasonic technology (HT) has been reported to significantly reduce serous drainage in superficial and total parotidectomy; thyroidectomy; tonsillectomy; pectoralis major myocutaneous flap dissection; axillary dissection; and lymphadenectomy. One of the authors' unpublished data in total lower body lifts using HT demonstrated a significant reduction in drainage compared to electrocoagulation (EC). The aim of this study was to determine if the use of HT in abdominolipectomy reduces volume and duration of postoperative wound drainage when compared EC.
Methods: A prospective, randomized, single blind, parallel group, multi-center study of the HT versus EC for tissue dissection and vascular control in abdominolipectomy was conducted by plastic surgeons located in Germany, Argentina, Mexico, and the U.S. After signing an informed consent, forty five adults scheduled for full standard abdominolipectomy were randomly allocated to undergo surgery with HT or EC. The group allocation was not revealed to the surgeon until after the induction of sedation/anesthesia. All statistical tests were based on two-side t-test at a significance level of a=0.05. All null hypotheses are stated as no difference in serous drainage volume and duration, and operative time between HT and EC.
Materials: The Harmonic™ consists of a generator, a hand piece with a connecting cable, and a sharp curved blade (Ethicon Endo-Surgery, Cincinnati, Ohio). Monopolar EC was used by all sites (different vendors). All sites used two 19F round Blake™ full fluted silicone drain with J-VAC bulb reservoir for suction of postoperative serious drainage (Ethicon Inc., New Jersey, NY,)
Experience: Forty five subjects (42 females and 3 males) were enrolled from October 2006 to February 2007 (14 in Germany, 11 in Mexico, 14 in Argentina, and 6 in the U.S.A.). There was no significant difference in demographic characteristics between the groups. The majority of subjects were either Hispanic (24) or Caucasian (20). No significant differences were observed in weight of excess tissue excised, type of postoperative compression, time to ambulation, and hospitalization time. Two closed wound drains were placed in all subjects intraoperatively and serous secretion was measured daily until volume was ≤50 mL/24 hour, at which time the drains were removed.
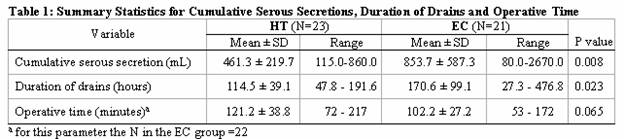
Summary of results: Serous secretion data were available in forty four subjects, 23 in the HT and 21 in the EC group (one subject was excluded from analysis due to noncompliance to post-operative care instructions). Table 1 summarizes the study result in terms of cumulative serous secretions, duration of drains and operative time.
Two cases of seroma requiring aspiration occurred with EC and one with HT. One mild hematoma was reported with HT and two with EC. One case of mild skin-flap ischemia was reported in the HT group but was not related to the device.
Conclusions: This study demonstrates that the use of HT in abdominolipectomies appears safe and, compared to EC, results in an almost 50% reduction in postoperative serous accumulation and a corresponding 2-day reduction in the use of closed suction drainage. There was a trend suggesting a longer average operative time with EC; however, this difference may be related to inexperience with HT as suggested by the finding that the one study site with previous HT experience reported similar operative times for both groups. Additional studies may be warranted to confirm these results and to investigate additional related outcomes such as healing, risk of retrograde infection, and patient comfort.
View Synopsis (.doc format, 149.0 kb)
See more of Technology Based
Back to 2007am Complete Scientific Program