Monday, October 29, 2007
12991
Computer Assisted Orthognatic Surgery Based on 3D Cephalometry. A New Approach with 3D Surgical Wavers
Purpose:
Computerization and sophisticated radiographic technology in orthodontics and orthognathic surgery have contributed immensely to the stockpile of knowledge. Another significant improvement can be attributed to the development of 3D visualisation software of radiological data and segmentation of anatomical defined objects. Although excellent navigation hardware and 3D planning software are available, there is still a need for tools featuring simple and rapid synthesis of both, the realization of a pre-surgically planned situation and the valid intraoperatively transformation. Several approaches to solve the problem of bony segment translocation with a navigation system have been already attempted (Troulis et al. 2002). Different approaches have to be made using the principles of augmented or virtual reality (Mischkowski et al. 2006).
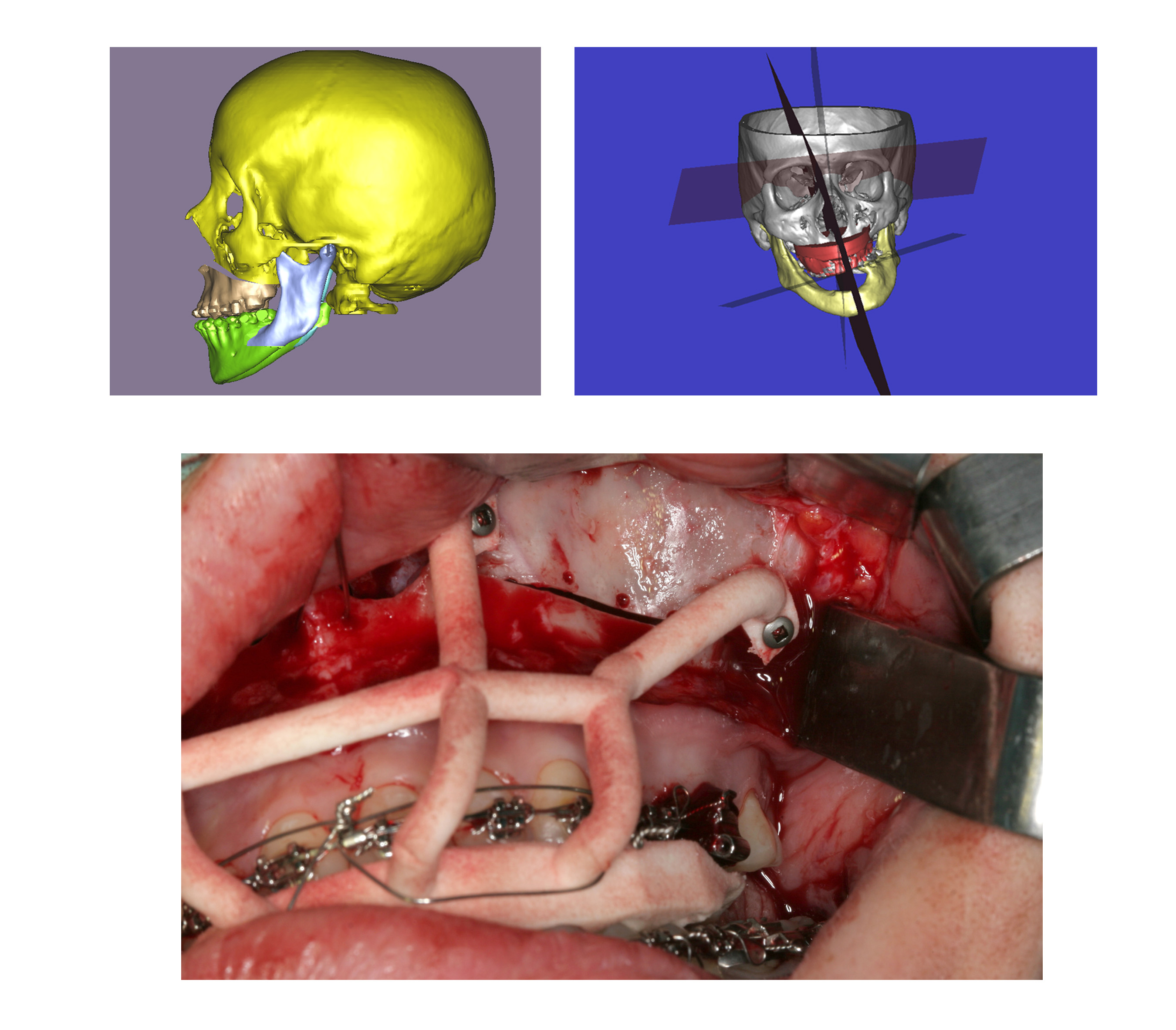
The purpose of this study is to introduce a new surgical waver concept (fig. 1) based on computer assisted surgery. The transformation of the presurgical information is doe with new designed surgical wavers. The novel surgical wavers were individually made in cooperation with Materialise Belgium, by means of stereolithography. A further goal of this study was the evaluation of the precision, reliability and feasibility of this new technique including the capability of soft-tissue prediction.
Methods:
This study contains 15 patients with orthognatic deformities (open bite, class II and class III). The orthognatic surgery planning was done preoperatively referring to anatomical landmarks (basal skull) as a reference plane. Perpendicular through the nasion the facial median-plane was created. These symmetrical planes represent the ideal facial situation. Based on these planes the surgical techniques were determined in order to get the best symmetrical result. Then surgical wavers have been developed to transfer the virtual planning. The major of this “new “ contains the surgical of the presurgical virtual planning as exact as possible as well as the repositioning of the centrical position of the temporo-mandibular-joint. Our surgical concept is based on 3 splints. The first waver is used to define reference holes in the segmented bone before the transposition was performed. After the osteotomies the second surgical waver fix the segmented bone in the new “desired virtual” position. For bimaxillary osteotomies the third waver fix the definitive occlusion and reposition the mandibular joint in the centrical position. To compare the achieved result the pre- and postoperativ CT or DVT dataset were fused.
Results:
The new 3D computer assisted approach was applied for orthognatic surgeries in 15 patients, 10 underwent bimaxillary osteotomies and 5 monomaxillary osteotomies. Maxillary retrognathia and mandibular prognathia was the diagnosis in 10 cases. One patient had in addition an open bite and 2 patients each had bimaxillary laterognathia 3 cases had mandibular prognathia and 2 cases mandibular retrognathia. The great advantage of these technique consists in the rigid fixation of the bone parts through the wavers. This facilitates the fixation of the osteotomy plates. The control or comparison group contained also 15 patients. The 3D-cephalometric analysis based on pre- and postoperatively CT or DVT data showed that the accuracy when using the “new surgical 3D splints” including the computer assisted approach was within a range of 1 mm of the surgical plan. In the control group (classical planning) the accuracy was within a range of 1,5 mm including a tendency to advance the maxilla less than the planned distance was noticed.
Conclusion:
Computer generated 3D-image prediction is suitable for patient education and communication. This simulation system will be particularly useful for the selection of an optimal operative method in cases in which change in facial soft tissue shape should be carefully deliberated. In the authors hand, the use of this new surgical templates has resulted in outcomes close to those predicted by the planning process. The “new 3D-splints” have the potential to become a valuable tool in orthognathic surgery. Up to now monomaxillary and bimaxillary osteotomies were evaluated. The application to other types of more complex osteotomies, including segment osteotomies are currently under investigation.
View Synopsis (.doc format, 3006.0 kb)
See more of Cranio/Maxillofacial/Head & Neck
Back to 2007am Complete Scientific Program
