Sunday, October 28, 2007
13526
Virtual Orthognathic Surgery: How Accurately Can One Plan a Procedure?
PURPOSE: The ability to use computer-based, virtual planning for orthognathic surgery is desirable for several reasons: it would allow the surgeon to easily simulate multiple different surgical approaches for a given case, to predict postoperative aesthetic outcome and dental occlusion, and to help minimize intraoperative errors in osteotomy design and in placement of the osteotomized segment(s). As such, software-based orthognathic simulation has been attempted to varying degrees. Recently, we have used such software in the planning of orthognathic procedures. It remains to be established however, how such surgical planning correlates with actual postoperative results. Patients with mandibular deficiency, maxillary deficiency, anterior open bite deformity, and facial skeletal asymmetry have been undergone orthognathic surgical correction followed by virtual planning.
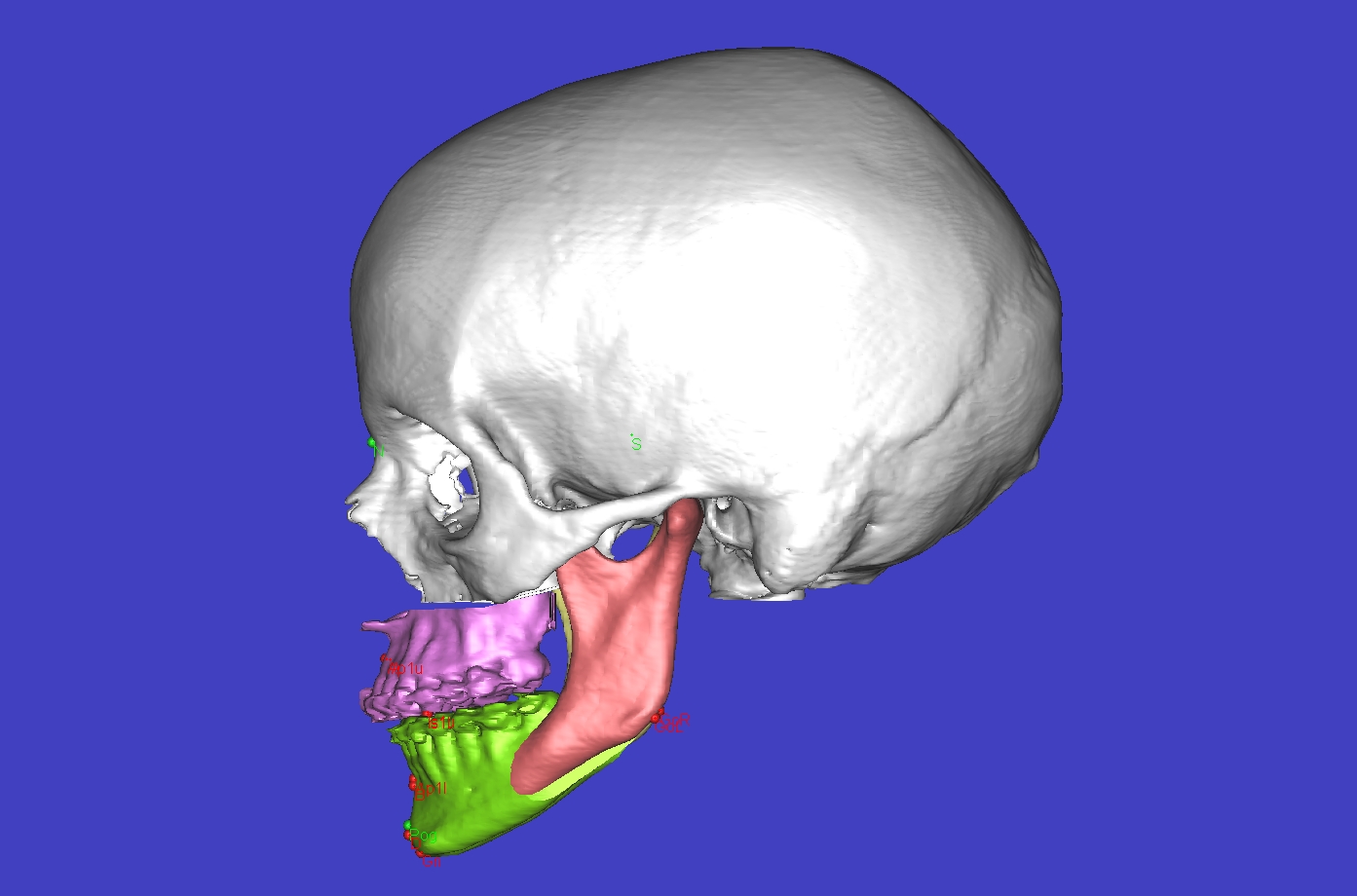
METHODS AND MATERIALS: For patients undergoing orthognathic treatment for either a congenital or developmentally-abnormal relationship of the jaws to the cranial base, both preoperative lateral cephalogram and CT scan of the facial bones are routinely obtained and DICOM data is imported into SIMPLANT Pro/CMF (Materilise, Belgian) software. Following segmentation, virtual osteotomy cuts are made and osteotomized segments positioned so as to achieve desired goals in occlusion and in facial skeletal harmony (FIGURE). A set of established cephalometric landmarks have been defined and preoperative Steiners analysis completed.
For patients who underwent single or double jaw surgery, osteotomies were made and segments positioned according to the virtual plan. Postoperative lateral cephalograms were obtained, corresponding landmarks identified, and their positions compared to those of both the preoperative cephalogram and CT.
RESULTS: Parallel and quantitatively similar movements were observed when comparing the change in position of cephalometric landmarks on postoperative cephalogram to the predicted position of the corresponding landmark by preoperative simulation.
CONCLUSIONS: Virtual surgery offers the possibilities of more accurate planning of orthognathic procedures, and a simpler way of considering multiple surgical approaches to achieve a result. Here we demonstrate both our center's current approach to using virtual surgery in planning such procedures and the means by which we quantitatively compare predicted skeletal bone movement to actual movement.
View Synopsis (.doc format, 659.0 kb)
