Sunday, October 28, 2007
13531
A Novel Model for Evaluating the Anatomic and Physiologic Effects of Rhinoplasty
PURPOSE: The relationships between nasal anatomy, physiology and function are complex. Even small changes in mucosal surface configuration (from infection, inflammation, trauma or surgery) can dramatically change the cross-sectional area of the nasal passageway and similarly the resistance. Several basic science and clinical studies have demonstrated the effects of nasal surgery subjectively but only to a limited extent objectively. These studies are limited by active changes in the mucosa, which muddle perioperative interpretation of the effects of surgery. Additionally, rhinoplasty often involves multiple procedures, making it difficult to isolate and evaluate the effects of independent maneuvers. The purpose of this study is to develop a robust cadaveric model of biphasic nasal respiration, unhindered by mucosal activity that allows objective evaluation of surgical procedures and their effects.
METHODS: Ten unpreserved heads (average age 73) were tracheally intubated, retrograde through the neck, such that the balloon obstructed the nasopharynx at the level of the soft palate. The oral cavity was obliterated using alginate and the lips were sutured together, thus isolating airflow from the nasopharynx to the nasal ala. Tissue quality was preserved by routine rehydration with isotonic fluid. Nasal airflow was simulated using three different methods (ventilator – sinusoidal flow, regulated wall suction – strong inhalation, and regulated wall air – strong exhalation). These encompassed all pressure-flow relationships from laminar and turbulent flow to the unsteady extreme of nasal valve collapse. Acoustic rhinometry and rhinomanometry were used in each nostril to evaluate the cross-sectional area, nasal resistance, and pressure-flow relationships in the native state and after each controlled surgical intervention.
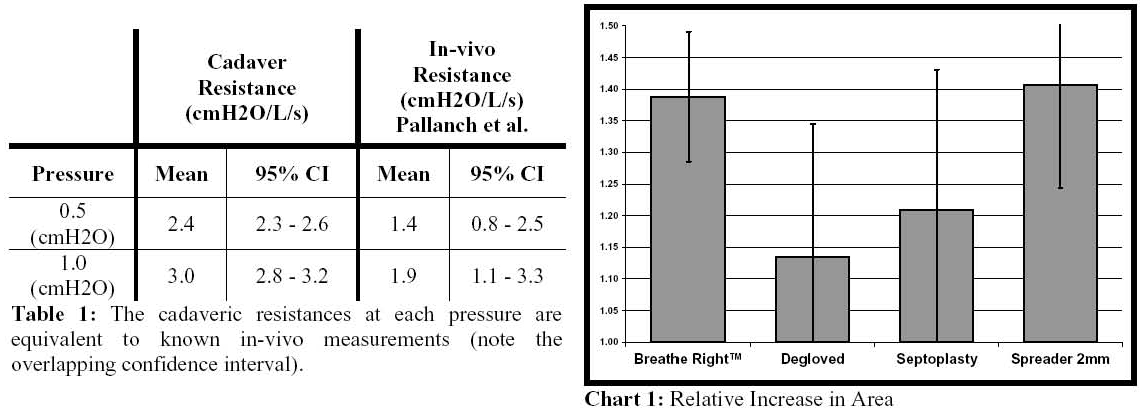
RESULTS: The average minimal cross-sectional area at the internal nasal valve was 0.91cm² (SD 0.2). At a pressure gradient of 0.5cmH2O across the nasal passage, the average resistance (cmH2O/L/s) was 2.47 (95CI 2.31, 2.62). At 1.0 cmH2O, the average resistance was 3.01 (95CI 2.79, 3.23) (Table 1). Measurements were repeated three times in each nare with an inter-measurement variability of <0.2%. Of the surgical maneuvers tested, a significant increase in cross sectional area (40%) was obtained with 2mm spreader grafts. Interestingly, a similar increase was noted with a Breathright™ strip (Chart 1).
CONCLUSIONS: This study completes the first step in objectively and quantitatively characterizing the physiologic effects of rhinoplastic procedures. The model is validated; it closely reproduces in-vivo nasal anatomy and physiology, allowing for the objective measurement of surgery on nasal airflow, resistance, and cross-sectional area without the complications of in-vivo mucosal fluctuations. The measured resistances and cross-sectional areas were consistent with age-adjusted in-vivo norms. This model provides a powerful tool for evaluating and comparing the isolated effects of various surgical techniques on the nose.
View Synopsis (.doc format, 37.0 kb)
