Friday, October 31, 2008
14467
NOVEL Shape of a Manibular Cutaneous Flap to Repair Cheek and Labial Facial Units(MCP)
NOVEL SHAPE OF A MANIBULAR CUTANEOUS FLAP TO REPAIR CHEEK AND LABIAL FACIAL UNITS(MCP)
The aim of this study is to demonstrate a novel shape of a cutaneous flap, designed on the facial angiossome supplied by the facial artery over the mandibular projection. The flap can replace soft tissue in the cheek and labial facial sub-units at the same time. It was indicated in the treatment of vascular malformation(3 cases) , complex pilousus nevus(2 cases) and burn scars(2 cases).
Method: With the patient under sedation, the MCP Flap is planned starting just 1.5cm from the auricular lobule running parallel to the mandibular border superiorly until a point 1.5 cm from the oral commissure. From this point, the line goes down to the mentum, returns 1cm parallel the inferior border of the mandibular projection inferiorly until the mandibular angle.(Fig 1) Tumescent infiltration using lidocaine 0,5% is utilized to easy the undermining over the SMAS plane. The donor site is closed primarily and the flap is rotated to the cheek and labial sub-unit as necessary. In 2 patients- 17 years-old and 22 years-old respectively, expander was indicated. (Fig 2,3) In the last ten years, 7 patients with ages varying from 17 to 50 years-old underwent to the procedure. In the total: 7 MCP flaps was indicated to treat 10 facial units. The follow-up range from six months to five years. (Fig. 4)
Results: The MCP replaced successfully the malar and labial units in six patients. In one case-a patient with a complex vascular malformation-, the labial sub-unit was replaced with Abbé flap.(Fig. 5). The post-operative period was uneventful. The first patient presented a hematoma.
Discussion: The mandibular flap delineated according the strategy of this study is located over the facial artery angiossome. The MCP can provide satisfactory tissue to replace adequately the malar and labial units. In selective cases, it is a better choice than the multiple stages of cervical flap advancement, because in this case it is more difficult to achieve a shape of facial unit, than with the MCP flap rotation. In young patients or those with inelastic skin, a previous expansion can be helpful. In those patients with good elasticity, a direct rotation without expansion can be done in one or two stages procedure. We have to give special attention during the flap design, preserving at a minimum 1.5cm from the labial commissure, in order to allow primary closure of the donor site, avoiding displace the oral angle. With the superior and inferior limit of the flap running 1cm from mandibular border, the flap area can reach 9-10cm in length by 3.5 -4.5 cm width. The indicaton of MCP flap is of importance in patients with vascular malformation not responsible to laser therapy, as well as the complex nevus involving two or more facial units. (Fig. 6, 7)
Conclusion:The mandibular cutaneous flap with the parameters proposed by the authors, can provide enough tissue to repair the homolateral malar and labial facial units, according preliminary clinical investigation
 .
.
Fig 1 – Design of the MCP Flap

Fig. 2a – Transoperative view of the MCP flap before rotation to cheek and labial facial units

Fig. 2b – The MCP Flap at the receptor site.

Fig. 3 – 5 year pos-operative view of the patient of fig. 2

Fig. 4 – The MCP flap after repair of the vascular malformation
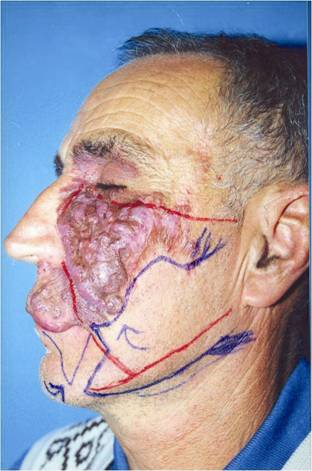
Fig 5a – The planification of the MCP flap to repair complex vascular malformation
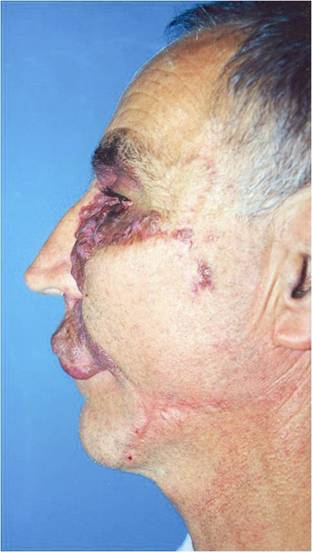
Fig 5b – The flap at the receptor site after the first stage
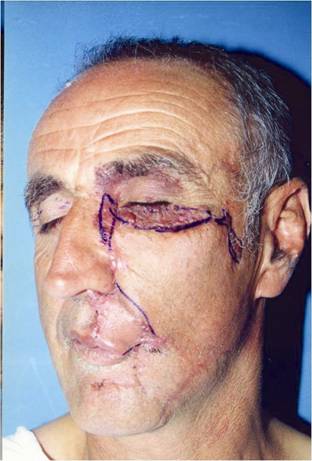
Fig. 6 – The MCP flap covering all the cheek unit and the Abbé flap correcting the homolateral orbicular unit

Fig. 7a – Preoperative view of a complex vascular malformation taking 3 facial subunits
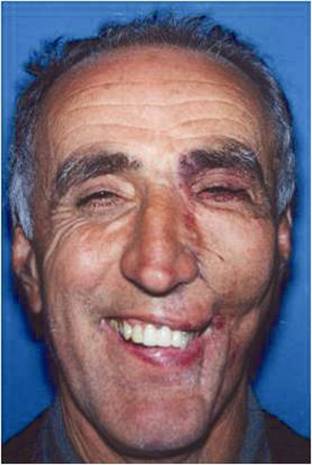
Fig. 7b – 1 year postoperative view of the MCP flap rotated to the cheek unit