Wednesday, November 5, 2008
14605
Vertical Reduction Mammaplasty: Quantification of the Learning Curve in One Hundred Consecutive Cases by a Single Surgeon
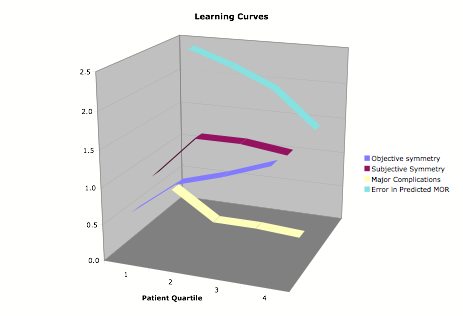
Background: Reduction mammaplasty utilizing a vertical scar and a superior or medial dermoglandular pedicle provides several widely accepted advantages over alternative techniques. Authors have often cited the "intuitive" nature and difficult learning curve of the technique as impediments to its widespread use. Here we seek to quantify the learning curve of this operation in an effort to determine the critical factors for mastering this powerful technique and minimizing complications. Methods: One hundred consecutive vertical incision breast reductions performed by a single surgeon were reviewed in an attempt to quantify the rate of improvement in several key objective and subjective outcome measures over time. Variables analyzed included patient demographic information, BMI, predicted and actual weight of resection, IMF repositioning, pre- and post-operative symmetry as measured both subjectively and objectively, pedicle choice, and rates of minor and major complications. The one hundred cases were divided into temporal quartiles for analysis of various performance measures as the senior surgeon gained comfort and familiarity with the technique. Data from the four quartiles were compared using the ANOVA and Mann-Whitney U tests for normally distributed non-parametric variables, respectively. Results: The mean pt age was 31 (range: 17-62) with a BMI of 24.8 (range 17.8-33.8). These parameters did not fluctuate significantly between quartiles. Postoperative improvement in breast symmetry (measured by both a subjective grading system and sternal notch to nipple-areola complex distance) and rates of major complications decreased in a statistically significant fashion from the first 25 cases to the last 25. There was no statistically significant change in minor complications (spit stitches, wound erythema, etcÉ) suggesting that these represent risks inherent to surgery. There was a marked improvement approaching statistical significance in the concordance between predicted and actual weight resected from the first quartile to the last. The senior author's refinements to this technique resulting in improved outcomes are presented including the necessity of preoperative skin/ glandular quality assessment, an algorithm for determining choice of pedicle, and adequate fixation of both gland and skin to control breast shape and position Conclusions: Quantitative learning curve analysis is becoming widespread in other surgical fields, as the pay-for-performance paradigm has taken hold. This study represents the first report of quantitative "single-surgeon" learning curve analysis in the plastic surgical literature. Our data clearly demonstrate that the "learning curve" of the v ertical scar technique can be quantified in terms of subjective and objective criteria. Continued analysis of outcomes is critical for identifying areas for constant refinement of technique, however detailed quantitative statistical analysis such as presented here can aid in determining an average number of cases necessary to attain safety and proficiency.