Monday, November 3, 2008
14701
Correction of Frontoethmoidal Encephaloceles: HULA Repair
Background: Frontonasoethmoidal encephalomenigoceles, rarely seen in the Western Hemisphere, remains a challenging clinical entity. This midline facial deformity involves a central herniation of a glial mass which ‘pushes outward' and deforms the medial orbit, medial canthus, nasomaxillary process and nasal structures without resulting in hypertelorbitism. The ‘Chula' repair, named after King Chulalongkorn of Thailand, and other techniques focus on extracranial resection and nasal dorsal reconstruction. In the HULA repair we describe resection of the deforming mass, repair of the cranial base defect and complete reconstruction of the midline hard and soft tissue structures.
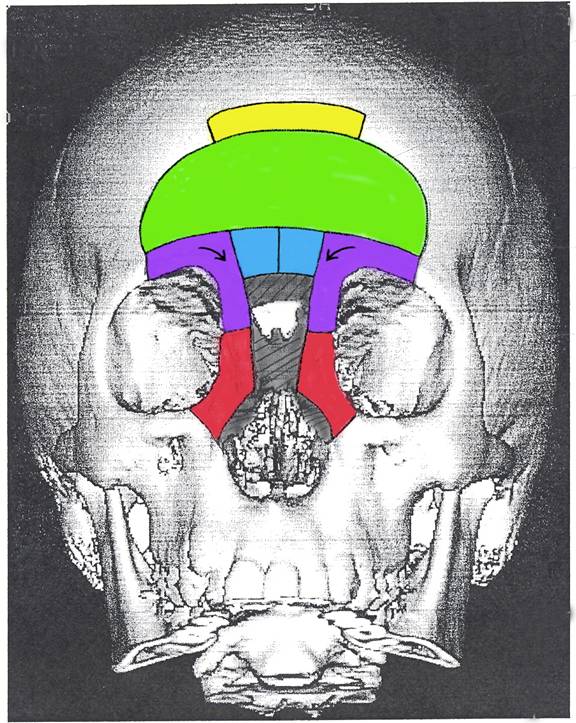
Methods: Filipino patients diagnosed with frontonasoethmoidal encephalomenigoceles were treated by a multidisciplinary team during joint civilian/military humanitarian missions at Tripler Army Hospital (n=12). Demographic, medical history and CT scan information was recorded. Operative technique evolved and varied slightly depending on the deformity but followed tenets of the HULA Frontoethmoidal Encephalocele Correction (Figure 1): H = Hard split cranial bone, pericranial flap, Fibrin Glue sealant after ligation of cyst stalk and dura repair; U = Unification of supraorbital bar after midline resection and inward rotation; L = Low nasal radix position for full thickness cantilever bone graft; A = Adjustment of medial canthal position and nasal maxillary process after resection of midline accessory nasal bone. Postoperative and follow-up assessment was based on examination, photographic images, CT scans, parental surveys, the Whitaker reconstructive score and developmental testing.
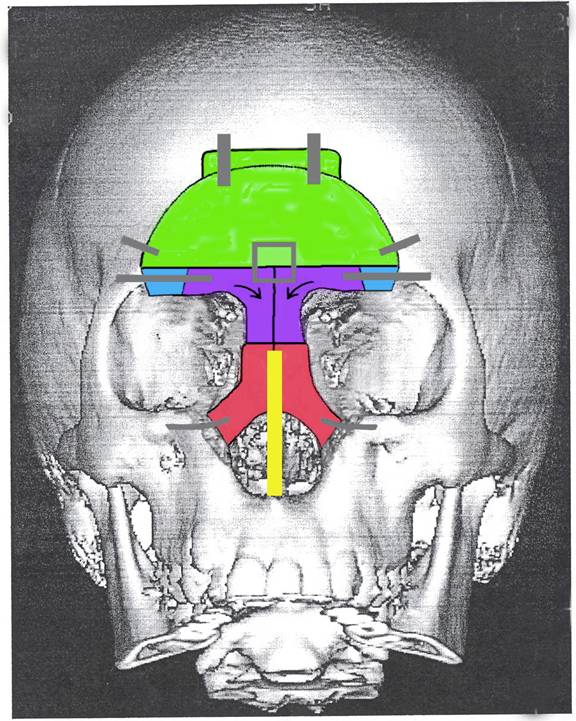
Results: Patients ranged in age from 5 to 12 years; there were 67% females and 33% males. All cases involved frontoethmoidal or nasoethmoidal defects. Sixty-six percent of patients underwent central nasal skin excisions of ‘damaged,' or poor quality, hyperpigmented skin. Patients with undamaged nasal skin did not require an external skin incision but instead had bilateral maxillary gingivobuccal sulcus incision for removal of the central mass. In these patients an intercartilagenous nasal incision was used to place the cantelever bone graft. After the HULA procedures no patients manifested cerebrospinal fluid leaks, infection, or elevated intracranial pressures. Follow up at 6 months-4 years revealed satisfactory correction of the deformities (mean Whitaker score of 1.3=no or minor soft tissue revision only necessary) (Figure 2). Parental survey showed very good to excellent aesthetic outcome with a high degree of satisfaction. Follow-up developmental tests showed normal scores in preschool tests (mean score=102) and global evaluations with normal memory and attention skills.
Conclusion: Our outcomes demonstrated that the HULA technique was a safe and effective approach to correct the complex craniofacial anomaly of frontoethmoidal encephalomenigoceles.