Tuesday, November 4, 2008
14722
Application of Poly-Dihydroacetate Bioadhesive Signficantly Reduces Post-Operative Seroma Formation in a Rat Mastectomy Model
Application of Poly-Dihydroacetate Bioadhesive Signficantly Reduces Post-Operative Seroma Formation in a Rat Mastectomy Model
Sunil P. Singh, BA, Peter Zawaneh, BS, David Putnam, Ph.D., Jason A. Spector, MD
Background: Seromas are common post-operative complications in both cosmetic and reconstructive surgery that, without timely intervention, may result in significant morbidity including disfigurement, pain, infection (which can be especially problematic when implants or other foreign materials have been placed) or even formation of permanent cystic cavities. They are especially common in ablative procedure, such as mastectomies, that require extensive dissection and create large surgical voids. Once present, seromas may persist despite repeated aspiration, resulting in distress for both patient and surgeon alike. Measures to prevent the formation of seromas, such as “quilting” sutures and use of fibrin or other biologic sealants, have been disappointing at decreasing the incidence of post-operative seroma formation.
We have developed a novel biocompatible and biodegradable injectable hydrogel based on polyethylene glycol and a polycarbonate of dihydroxyacetone (PEG-pDHA). This polymer has significant bioadhesive properties; it is fabricated from compounds naturally derived from the human body (DHA) and is broken down to natural body byproducts including carbon dioxide and water. Unlike current tissue sealants, which bind to tissue with a low binding constant, our polymer reacts covalently through the formation of a Schiff-base, resulting in a binding constant of 1015 M-1. This study set out to determine the in vivo efficacy of our novel compound in preventing the formation of seroma in a rat mastectomy model.
Methods: This study used a previously described rat mastectomy model to induce seroma formation. Fifteen male Sprague-Dawley rats (9 experimental, 6 controls) underwent the procedure. Starting with a midline incision, a skin flap was raised over the right chest, the right pectoralis major muscle was excised and a right axillary lymphadenctomy performed under an operating microscope. Experimental rats received 0.5cc of polyDHA into the wound bed before closure while controls received 0.5cc of saline into the wound bed before closure. Animals were sacrificed on post operative day #7 by carbon dioxide asphyxiation followed by cervical dislocation. Seroma fluid was aspirated percutaneously via 18 gauge needle and measured. The incision site was then opened and inspected for adhesions and any additional fluid remaining was removed by needle aspiration. Biopsies of the skin flap and underlying wound bed were sent for histologic analysis based on. In order to determine in vivo biocompatibility of the polymer, sections were analyzed for evidence of inflammation in the area of application. Seroma accumulation (total volume) was analyzed using the unpaired student's t test.
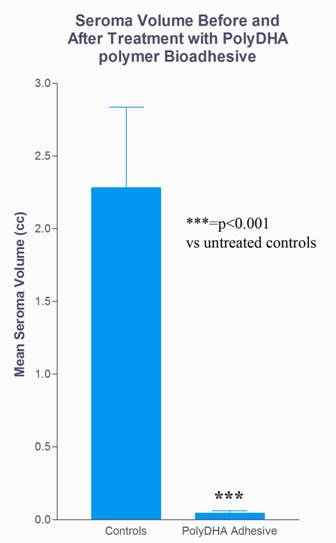
Results: Poly-DHA treatment resulted in a 98% decrease in seroma accumulation (mean volume=0.04cc) versus controls (mean volume=2.28cc) (p<0.001; Fig 1). Gross adhesions were seen between the skin flap and chest wall in the poly-DHA group while none were seen in the control group. Histologic examination demonstrated no evidence of increased inflammation reaction in poly-DHA treated animals versus controls. There were no differences in fibroplasia, inflammatory cell infiltration or neovascularization, all of which are consistent with normal changes in early stages of wound healing.
Conclusion: Our in vivo data demonstrates that our novel polymer, poly-DHA, has considerable bioadhesive properties, resulting in a significant reduction in seroma formation after mastectomy. Because our polymer is extremely efficacious, inexpensive and free of infection risk, we anticipate tremendous translational application of our novel compound in the realm of plastic and reconstructive surgery.
Figure 1: