Sunday, October 3, 2010 - 9:55 AM
17153
Safe and Effective Autologous Fat Graft Augmentation of the Upper Lid Sulcus: An Anatomic and Clinical Approach to Rejuvenation
Introduction
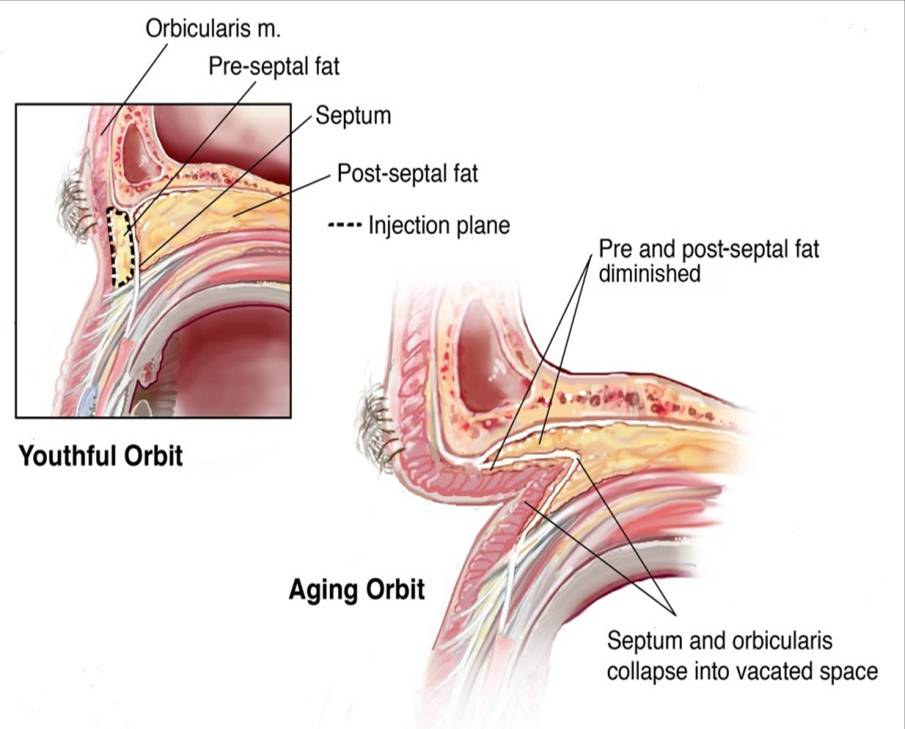
Characterization of the subcutaneous fat compartments of the face provided a possible mechanism for differential loss of volume in the aging face.1,2 We recently presented the senior author's experience in 452 female patients undergoing autologous fat augmentation in the face, focusing on fat loss in the mid- and lower face.3 Fat grafting has been employed to correct enophthalmos, though intraorbital injection is associated with a higher risk of fat embolus. To refine this approach we undertook:
1. Cadaver study to demonstrate a method to fat graft the superior eyelid sulcus for rejuvenation, with preservation of the integrity of the orbital septum to the reduce risk of intraorbital injection of fat.
2. Dissection to determine the fate of this fat anatomically after injection, and qualify the potential risk to the globe and periorbita.
3. Clinical application of these techniques, with longterm follow-up. Analysis and video of the technical aspects of the procedure is presented, with anatomic subtypes and potential pitfalls addressed.
Materials and Methods
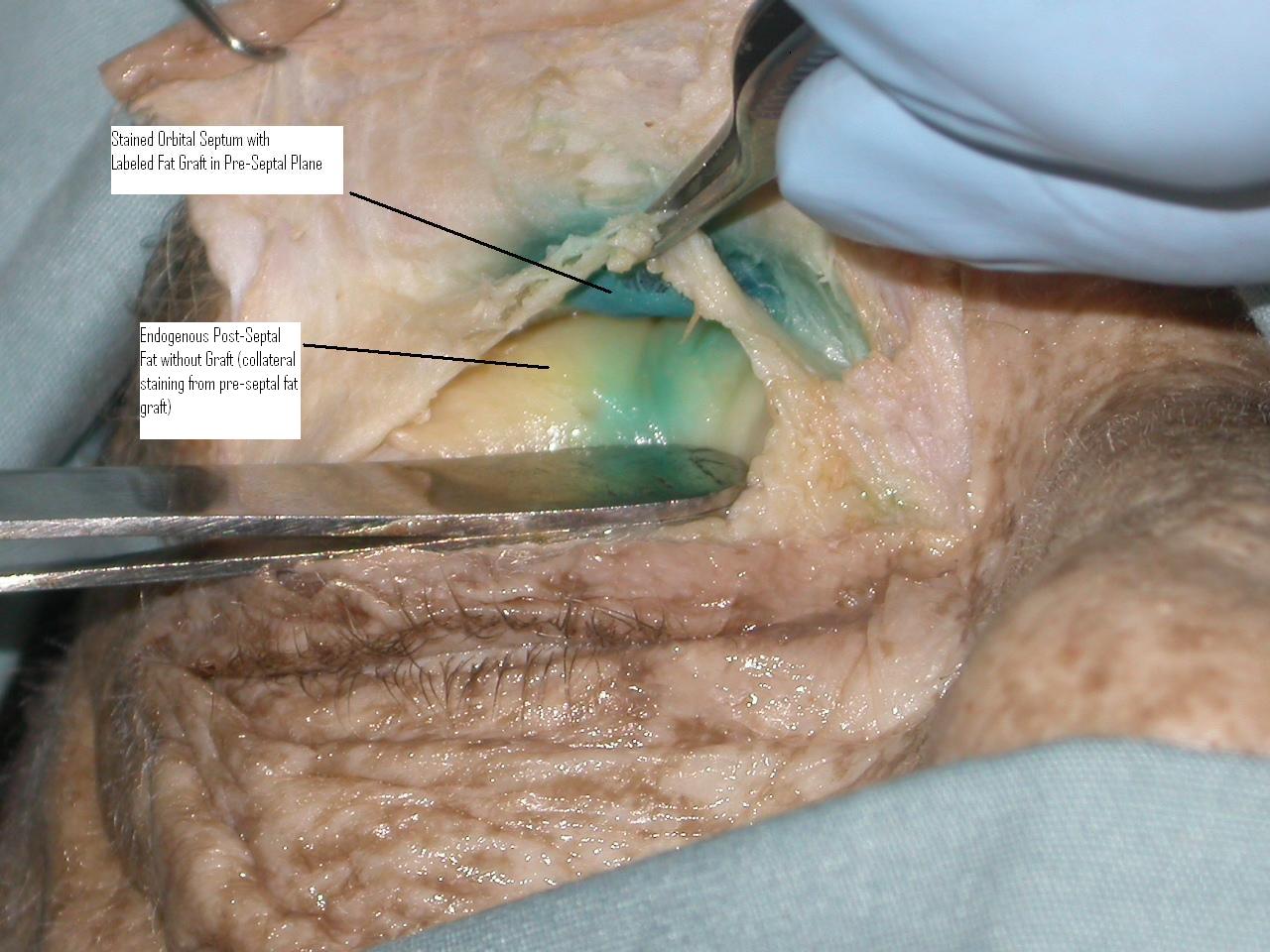
Periumbilical fat was harvested from consenting patients via suction syringe technique and labeled with methylene blue prior to injection into cadaver specimens, using a 17 gauge fat grafting cannula. Dissection then determined the exact anatomical location of the labeled fat. Photo-documentation was used to analyze and compare results.
A retrospective chart review of the Senior author's experience between September 2006-October 2008 was conducted. Periumbilical fat was harvested, processed, and placed superficial to the periosteum of the supraorbital rim, and in a preseptal plane. Patients were assessed by serial clinical photographs.
Results
Cadaver dissection uniformly demonstrated that injected fat was deposited in the retro-orbicularis oculi fat (ROOF) pad, without postseptal extension.
Forty upper eyelids in twenty-one consecutive female patients were treated for deepened suprapalpebral sulcus. Mean age was 56.6 years, and volumes injected were 0.20 to 2.30 cc per eyelid. Several patients had undergrafting, which was treated with repeat fat grafting or soft-tissue fillers, which is addressed as a complication. No hemorrhage, visual disturbances, infections, overgrafting or fat contour irregularities occurred.
Discussion
1. Fat grafting of the upper eyelid sulcus can be safe and reproducible with
meticulous technique and knowledge of the critical anatomy.
2. Preseptal fat placement may decrease the risk of periorbital injury and maximize aesthetic outcomes.
References
- Rohrich R. and Pessa J. The Fat Compartments of the Face: Anatomy and Clinical Implications for Cosmetic Surgery. PRS, Volume 119, Number 7, June 2007, pp 2219-2227.
- The anatomy of suborbicularis fat: implications for periorbital rejuvenation. Plast. Recon. Surg. September 2009, Vol. 124(3), 946-51.
- Sullivan PK, Hoy EA, Chang J. Liposculpture and fat grafting in the face and neck: A volumetric approach to rejuvenation. Plast. Recon. Surg. October 2009, Vol. 124, Issue 4S, 55.
- Hardy T., Joshi N., Martin K. Orbital Volume Augmentation With Autologous Microfat Grafts. Ophthalmic Plastic and Reconstructive Surgery, Volume 23, November/December 2007, pp 445-449.
- Trepsat F. Periorbital rejuvenation combining fat grafting and blepharoplasties. Aesth. Plast. Surg. 27: August 2003, 243-253.
See more of Cosmetic Paper (5 mins)
Back to 2010am Complete Scientific Program