Saturday, October 2, 2010 - 8:30 AM
18064
Quantitative Analysis of Vascular Response After Mandibular Fracture Repair Utilizing Micro-Computed Tomography with Vessel Perfusion
Purpose: Poor or delayed wound healing after mandibular fracture (Mfx) can be a devastating morbidity with significant clinical consequences. As angiogenesis plays an integral role in fracture healing, elucidating the angiogenic response after Mfx may help determine potential areas for therapeutic interventions. To date, the angiogenic response to Mfx is poorly documented and relies heavily on vague extrapolation from the endochondral literature. We have previously demonstrated the utility of high resolution, 3-D Micro-Computed Tomography (mCT) imaging in combination with vessel perfusion as a validated, quantitative, and objective method to assess mandibular vascular networks. We hypothesize that quantitative measure of vascular response after fracture healing in the membranous, highly cortical, mandible will return to normal levels soon after bony union, mirroring the results of endochondral, highly trabecular, long bones.
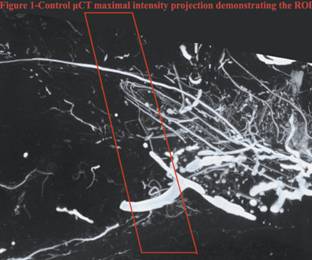
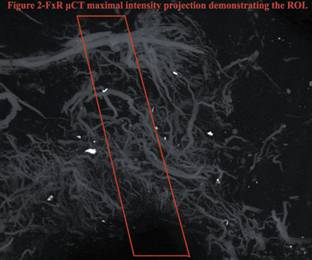
Methods: 12 Sprague-Dawley rats underwent left vertical ramus osteotomy and a 2mm fixed gap was set with an external fixator. Animals were sacrificed 40 days after surgery and Microfil was perfused into the vasculature. Specimens were decalcified and scanned with mCT at 18μ voxel size. The region of interest was analyzed for vessel volume, vessel volume fraction, vessel number, vessel thickness and vessel separation. The data was compared to an established non-fractured control. Analysis was conducted via ANOVA and post-hoc Tukey with statistical significance at p£0.05
Results: Stereological analysis demonstrated no statistically significant differences in the Mfx vasculature when compared to control animals. Our quantitative measures were as follows: vessel volume (1.716 mm3 vs. 1.668 mm3, p = 0.914), vessel volume fraction (0.028 vs. 0.032, p = 0.644), vessel number (0.497 mm-1 vs. 0.472 mm-1, p = 0.808), vessel thickness (0.052 mm vs. 0.067 mm, p = 0.191) and vessel separation (2.344 mm vs. 2.081 mm, p = 0.589).
Conclusion: To our knowledge this is the first study of vascular analysis of Mfx utilizing mCT after perfusion. Our findings indicate that vascularity returns to pre-fracture levels soon after union of Mfx. These results confirm our hypothesis, corroborate the findings in long bones, and solidify the application of mCT vascular analysis as an objective metric for measuring vascular response. Our results can now serve as a quantitative comparison for future experimentation regarding optimization of fracture repair in the cases of delayed healing as well as non-union.
Figure 1-Control μCT maximal intensity projection demonstrating the ROI.
Figure 2- FxR μCT maximal intensity projection demonstrating the ROI
See more of Cranio/Maxillofacial/Head and Neck Paper (5 mins)
Back to 2010am Complete Scientific Program