Monday, October 4, 2010
17352
Fluid Considerations to Minimize Early Postoperative Complications in Free Flap Breast Cancer Reconstruction
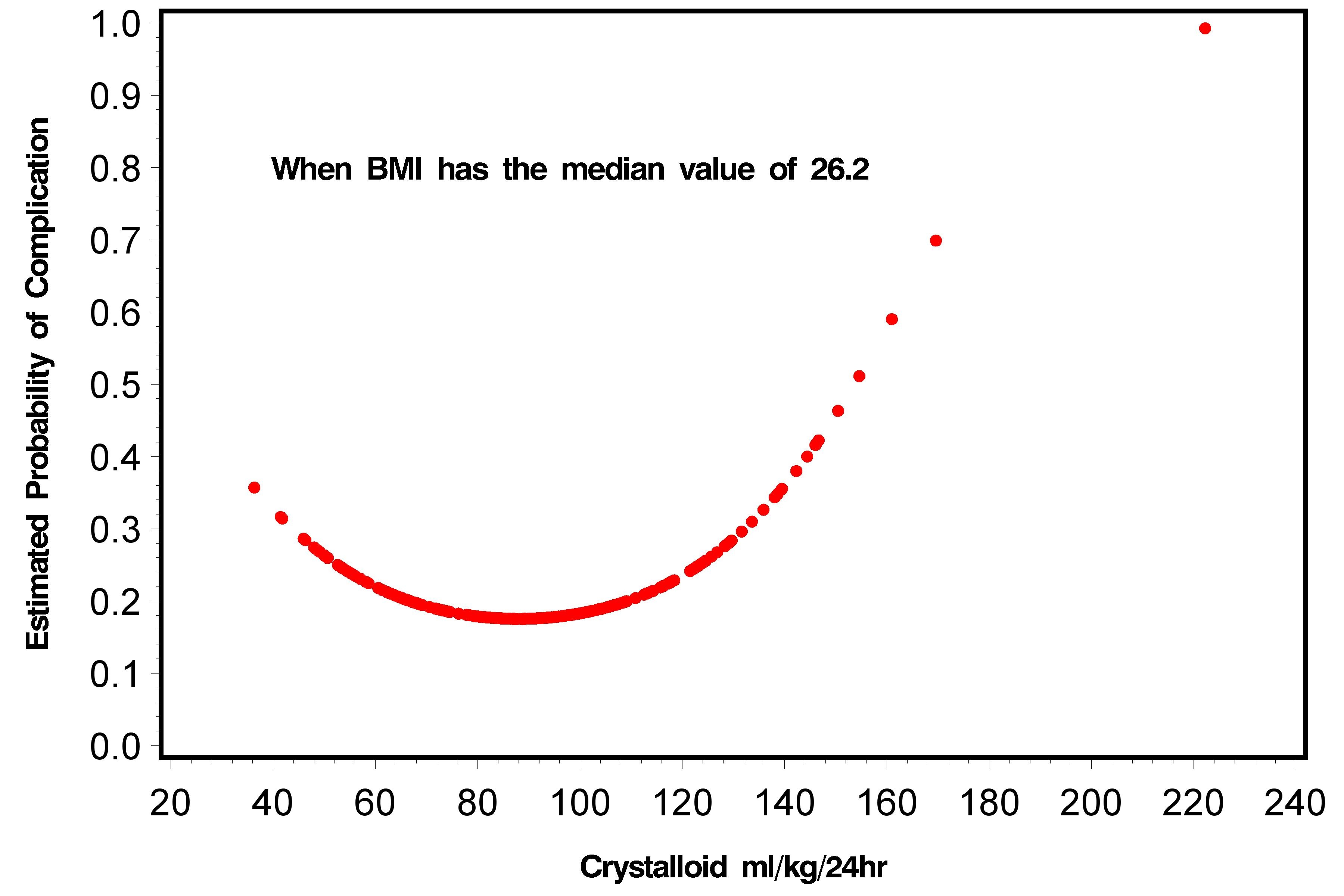
Purpose: Breast reconstruction has proven to be a safe and reliable procedure that does not compromise oncologic outcomes. An important aspect of free flap breast reconstruction that has not been previously studied pertains to the perioperative anesthetic and fluid management of these patients. Thus the purpose of thus study is to assess if there is an association between these factors with postoperative complications in patients undergoing free flap breast reconstruction. Method: A retrospective review was performed for the period between 2002 and 2009. All consecutive patients with free flap reconstruction of the breast following mastectomy performed at the University Health Network (Toronto,Canada) were identified in a prospectively maintained breast reconstruction database. Perioperative anesthetic variables analyzed included: BMI, ASA, preoperative hemoglobin, hematocrit, creatinine levels, and intraoperative colloid infusion rate/kg, crystalloid infusion rate/kg, and total fluid volume infusion rate/kg. Primary clinical outcomes included all minor and major post-operative complications. Results:In total, 285 patients received a total of 375 free flap reconstructions of the breast with one of four surgeons (TZ,SH,JL,PN) with a minimum of six-month follow up. Univariate analysis revealed both total volume of fluid infusion rate/kg (p = 0.015) and crystalloid infusion rate/kg (p = 0.013) during the surgery were significant independent risk factors for postoperative complications. Our final multivariate regression model showed that after controlling for the type of flap used (DIEP vs. free TRAM vs. other flaps) and effect of other covariates such as presence of a cardiac risk factor, both BMI and amount of crystalloid infused/kg were all significantly related to postoperative complications(p = 0.0448 and 0.0207 respectively). Furthermore, we found that a statistically significant quadratic relationship existed between the rate of peri-operative fluid infusion and risk of complication. Outside of the middle range of infusion rates, on either the low or high ends, higher risk of complication was observed. Conclusions: This is the first study to show that perioperative fluid management is related to post-operative complications in breast free flap surgery. Figure 1. Parabolic relationship between crystalloid infusion rate and complications when BMI is set to the median value of 26.24
See more of Hand & Upper Extremity (5 mins)
Back to 2010am Complete Scientific Program