Monday, October 4, 2010
18324
Use of Bioelectric Dressings for Faster Wound Healing: A Prospective Case Series
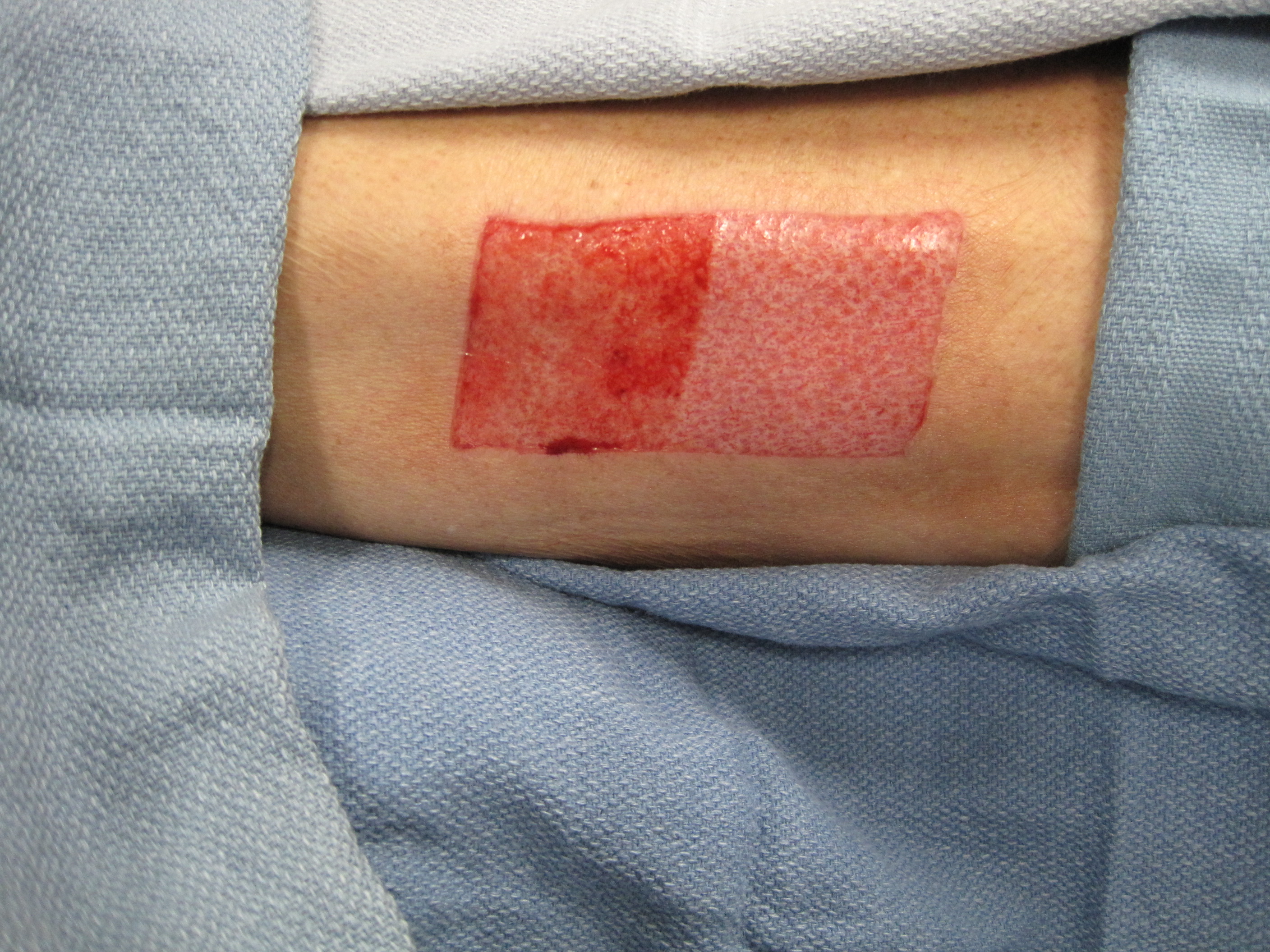
PURPOSE Despite advancements in wound care treatments for the management of acute and chronic wounds, there is an unmet need for interventions that accelerate epithelialization. Recent research findings support the use of bioelectric wound dressings to address this challenge (1-3). The principal aim of this study is to evaluate the impact of a bioelectric wound dressing on acute wound healing. METHODS Thirteen participants presenting to a multidisciplinary burn clinic were enrolled. Each patient underwent split-thickness skin graft (STSG) for treatment of their burn wound, with their donor site serving as the wound addressed for this study. STSG donor sites are the ideal control wound as they are of relatively uniform depth and have square margins for simple application of dressings. Each participant serves as his/her own control; one-half of all wound sites were treated with the bioelectric dressing and semi-occlusive dressing, the other half using solely semi-occlusive dressing (SOD). At each standardized follow-up visit, percent epithelialization and scar quality of wounds was rated by the same attending burn surgeon who served as a blinded evaluator. Localized pain was recorded using a Numeric Pain Intensity Scale. At monthly follow-ups, participants provided a self-assessment of their scar appearance. RESULTS At week 1 post-procedure, average epithelialization of 71.8% (SD=0.29) was noted on the bioelectric dressing treated side, compared to 46.9% (SD=0.33) on the SOD side, representing an average 52.95% faster wound healing. At week 2, participants indicated an average 39.44% decrease in pain scores on the bioelectric-treated wound half (bioelectric mean =1.3 SD=2.1, SOD mean =2.1, SD=2.9). At the one month scar evaluation, participants reported a decrease in scar pain, pruritis, scar color difference, scar stiffness, and scar thickness, and improved overall scar appearance on the bioelectric dressing treated half compared to the standard of care side, based on self-assessment. CONCLUSION This early data shows promise in terms of faster healing, improved scarring, and improved patient outcome with the use of the bioelectric dressing on acute wounds. With fulfillment of an extended study population, we hope to provide a solid foundation for extrapolating our data beyond skin graft donor sites to all areas of wound care. REFERENCES 1. Davis SC, Gil J, Valdes J, Perez R, Rivas Y. Assessment of the effects on wound healing and gene expression of a bioelectric dressing using a porcine wound model and real time reverse transcriptase-polymerase chain reaction. J Am Acad Dermatol. 2009;60:AB200. 2. Parker, I, Ho, A. The Treatment of Partial Thickness Burns with a Bioelectric Dressing Following Cosmetic Laser Facial Resurfacing. [abstract] J Burn Care Res 2009;30,2:AB171. 3. Sheftel SN. The role of a bio-electric, antimicrobial dressing in the healing of acute and chronic wounds [abstract]. Clinical Symposium on Advances in Skin and Wound Care, Las Vegas, NV. October 2008; (suppl): 217.
See more of Research (5 mins)
Back to 2010am Complete Scientific Program