Room 2 (Henry B. Gonzalez Convention Center)
Sunday, November 3, 2002
8:00 AM - 4:00 PM
Room 2 (Henry B. Gonzalez Convention Center)
Monday, November 4, 2002
8:00 AM - 4:00 PM
Room 2 (Henry B. Gonzalez Convention Center)
Tuesday, November 5, 2002
8:00 AM - 4:00 PM
Room 2 (Henry B. Gonzalez Convention Center)
Wednesday, November 6, 2002
8:00 AM - 4:00 PM
1068
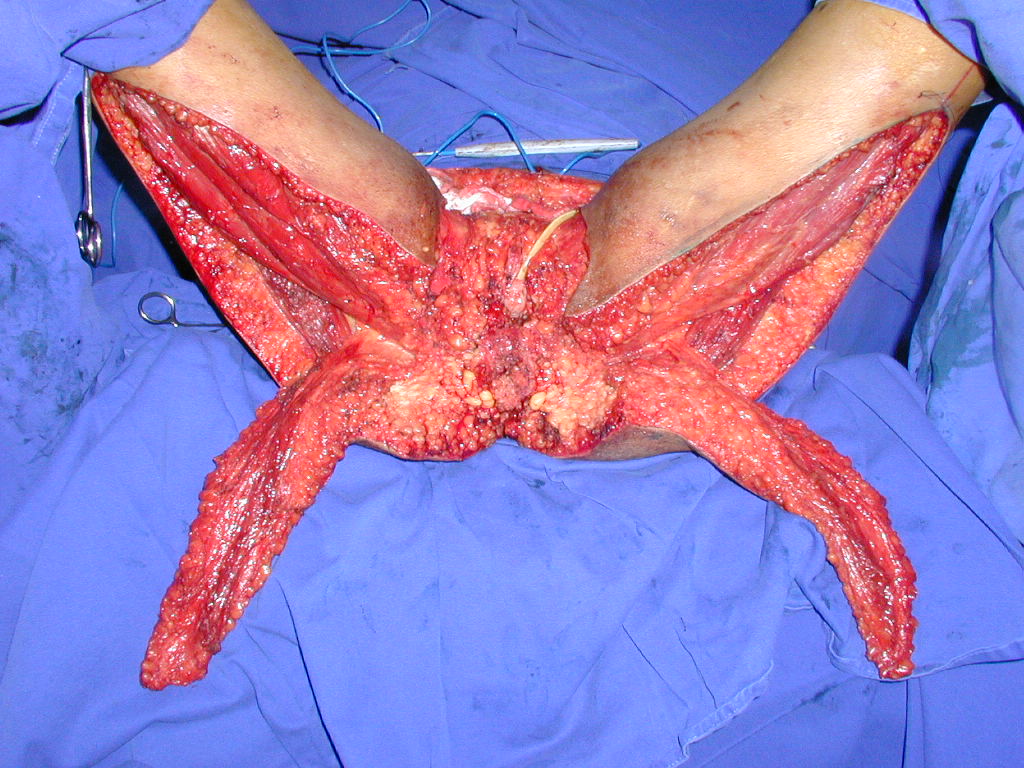
P56 - The Gluteal Thigh Flap - An Anatomical Study and Clinical Applications
The gluteal thigh (GT) flap was described by Hurwitz in 1980 for perineal and ischiatic reconstructions. It is a fasciocutaneous flap based in the descendent perforant branch of the inferior gluteal artery. This pedicle runs parallel to the posterior thigh cutaneous nerve. The aim of this study was to do an anatomical study in cadavers to establish landmarks to flap dissection and to show the viability to microsurgical transfer. Also, our clinical experience is presented. Thirty posterior thigh regions of fresh cadavers were used in this study. The collected data was: the distance between the divergence point of the biceps femoralis (BF) and semitendinous (ST) muscles until the popliteal crease; the distance of the vascular pedicle in the inferior verge of gluteus maximus (GM) muscle and the ischiatic tuberosity (IT); the extension of vascular pedicle and the relationship with the sciatic nerve (SN) and the posterior thigh cutaneous nerve (PTC); the diameter of pedicle on the inferior verge of the gluteus maximus muscle and the thickness of the flap. The results are presented in the Tables 1, 2 and 3. In the clinical study the gluteal thigh flap was used in 14 pressure sores, 7 vulvar reconstructions (Figures 1, 2 and 3) and 2 scrotum reconstruction. One flap (4.3%) had a partial loss of less than 10 %. No other major complications had occurred. Our results showed a constant anatomy, and similar skin characteristics to the nearby regions, favoring the reconstruction of the pressure sores and vulva, especially by the sensitive innervation of the flap. The recognizable extension of the pedicle was about 23 cm, therefore assuring an axial pattern of the flap. Due to the diameter the pedicle, it may be transferred microsurgically. The only major complication was due to the extreme length of the flap (40 cm). In our experience the gluteal thigh flap is a very reliable and easy to dissect, representing a good choice for ischiatic and perineal reconstructions.
| RESULTS | MEAN | STANDARD DEVIATION |
| Distance between the pedicle and IT | 4.71 cm | ±0.90 cm |
| Distance from the divergence point of BF muscle and ST muscle until popliteal crease | 12.07 cm | ±1.43 cm |
| Extension of pedicle | 23.12 cm | ±3.06 cm |
| External diameter of the perforant branch of the inferior gluteal artery | 1.13 mm | ±0.47mm |
Table 1- Results of the pedicle characteristic (n=30).
| DEPTH OF THE SCIATIC NERVE | MEAN | STANDARD DEVIATION |
| In the IT level | 1.71 cm | ±0.70 cm |
| In the the divergence point of BF muscle and ST muscle | 1.91 cm | ±0.64 cm |
Table 2- Relationship of the gluteal thigh flap pedicle and sciatic nerve (n=30).
| THICKNESS | MEAN | STANDARD DEVIATION |
| Subcutaneous at the IT level | 1.06 cm | ±0.60 cm |
| Subcutaneous distal at the divergence point of BF muscle and ST muscle | 0.66 cm | ±0.42 cm |
| Dermis and epidermis | 0.99 mm | ±0.60 mm |
Table 3 – Skin characteristics of the gluteal thigh flap (n=30) Figure 01.
Figure 02
Figura 03.
View Synopsis (.doc format, 585.0 kb)
See more of Posters
Back to 2002 Complete Scientific Program
Back to 2002 Meeting home