Room 2 (Henry B. Gonzalez Convention Center)
Sunday, November 3, 2002
8:00 AM - 4:00 PM
Room 2 (Henry B. Gonzalez Convention Center)
Monday, November 4, 2002
8:00 AM - 4:00 PM
Room 2 (Henry B. Gonzalez Convention Center)
Tuesday, November 5, 2002
8:00 AM - 4:00 PM
Room 2 (Henry B. Gonzalez Convention Center)
Wednesday, November 6, 2002
8:00 AM - 4:00 PM
447
P70 - Vulvar Reconstruction with Modified Fasciocutaneous Pudendal-Thigh Flaps
PURPOSE Vulvar reconstruction after cancer resection needs a reliable flap significant in terms of function. This flap must be thin, with a good vascular supply, providing sensation and a good cosmetic outcome. The purpose of this paper is to present a modified design of the fasciocutaneous pudendal-thigh flap.
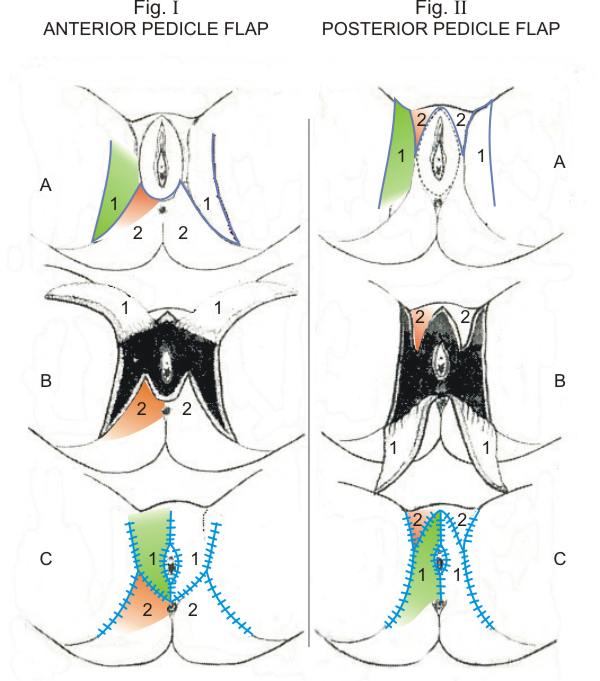
MATERIALS AND METHODS From June 2000 to February 2002 seven vulvar reconstructions were performed consecutive to vulvar cancer resection. The design of the flap was based on two principal vascular pedicles: the anterior one was the deep branch of the external pudendal artery, branch of the femoral artery and the posterior pedicle: the superficial perineal artery, branch of the internal pudendal artery. Both arteries supply a superficial vascular plexus above the fascia. The design of the flap is like an asymmetrical Z-plasty, with a long distal limb and a short proximal one. The bigger triangular flap must include the principal neuro-vascular pedicle so as to choose an anterior or posterior pedicle, based on the location of the lesion and the lymph-node dissection.A schematic representation of both flaps is showed (Fig I ,Anterior Pedicle Flap and Fig. II ,Posterior Pedicle Flap)where the small flap (2,orange)remains still and the big one(1,green)) is transposed to achieve a vulvar reconstruction.
EXPERIENCE A bilateral flap was transferred in each of five vulvar reconstructions and a unilateral flap was transplanted in 2 cases. In six cases the posterior pedicle was the choice and in one case an anterior pedicle flap was performed The smallest flap was 5 x 8 cm. and the largest 8 x 16 cm. In all the cases the diagnosis was squamous cell carcinoma.
RESULTS All flaps survive completely. Immediate postoperative complications occurred only in one patient that showed a breakdown of the suture caused by infection. She underwent to a delayed suturing. The functional and aesthetic results of all the patients were good.
CONCLUSIONS: A modified pudendal-thigh flap is presented. The design of a modified Z-plasty allows a better transposition and closure of the flap including the neuro-vascular pedicle.
View Synopsis (.doc format, 75.0 kb)
See more of Posters
Back to 2002 Complete Scientific Program
Back to 2002 Meeting home
