Wednesday, October 13, 2004 - 7:05 AM
5829
The Gastrocnemius-Achilles Tendon Myocutaneous Flap (GAT Flap) for Single Stage Reconstruction of Combined Soft Tissue and Extensor Mechanism Defects of the Knee: An 18 Year Experience
Purpose: This study retrospectively reviews our eighteen year experience with the Gastrocnemius-Achilles Tendon Myocutaneous Flap (GAT Flap). This represents a method for single stage reconstruction of soft tissue defects of the knee combined with loss or destruction of the underlying extensor tendon mechanism.
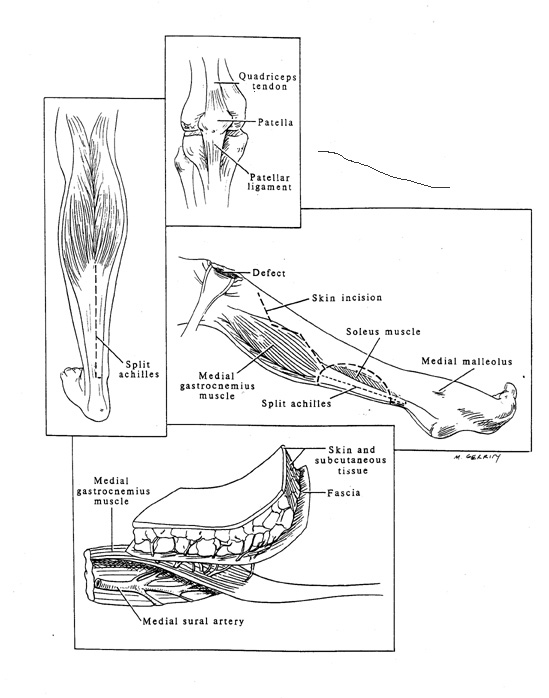
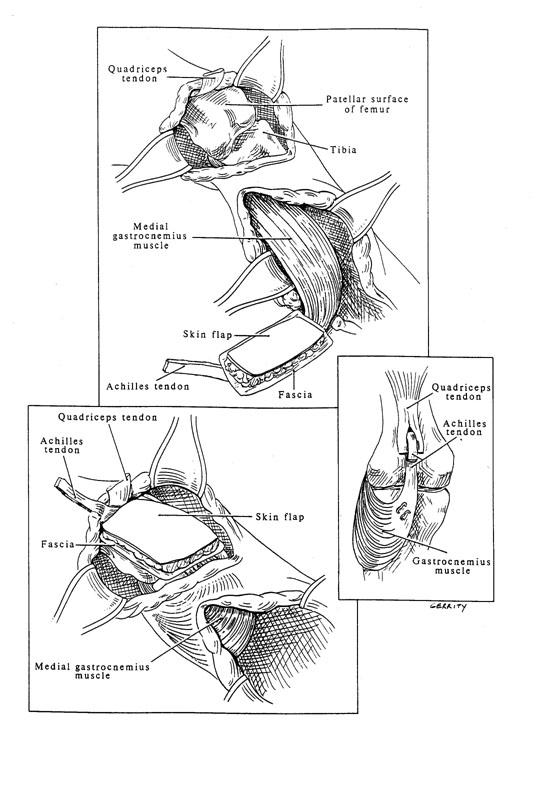
Materials and Methods: The GAT Flap, based upon the medial sural artery, is comprised of the medial gastrocnemius muscle, the medial one-half of the Achilles tendon, and the overlying fascia and skin. The deep fascia of the muscle and the proximal Achilles tendon are anchored to the tibia, the distal Achilles tendon is secured to the quadriceps mechanism, the fascial component reconstructs the knee capsule, and the skin paddle replaces the cutaneous deficit. The donor site is closed with a stsg. Seven patients underwent reconstruction with a GAT Flap. Indications included; complications after total knee arthroplasty (3), defect from trauma (3), and defect after tumor resection (1).
Results: All flaps survived although distal skin loss (<2 cm.) occurred in two patients. Five patients re-established excellent knee extension and strength. Four patients healed without complication. Donor site morbidity was minimal with uncompromised ankle function. Conclusions: Most soft tissue defects of the knee can be closed by well-described methods of reconstruction. However, the loss of soft tissue, compounded by the loss or destruction of the patella and underlying extensor tendon mechanism presents a more complex problem of functional restoration. This report describes the Gastrocnemius-Achilles Tendon Myocutaneous Flap (GAT Flap). The GAT Flap offers vascularized tendon transfer, knee joint capsule reconstruction, and gliding skin coverage in one stage. The GAT Flap re-establishes knee extension using a vascularized tendon. It provides single stage coverage of soft tissue defects of the knee while maintaining continuity of the extensor complex with its transposed tendon. The GAT Flap should be considered when reconstruction necessitates soft tissue closure and extensor mechanism reconstruction.
Figure 1
Figure 2
See more of General Reconstruction
Back to 2004am Complete Scientific Program