Sunday, October 10, 2004
5975
Botulinum Toxin (BT) Infiltration for Pain Control after Mastectomy and Subpectoral Tissue Expansion
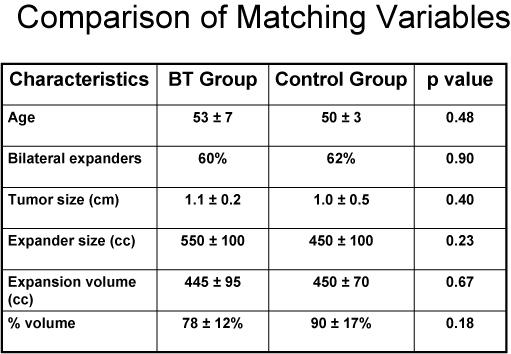
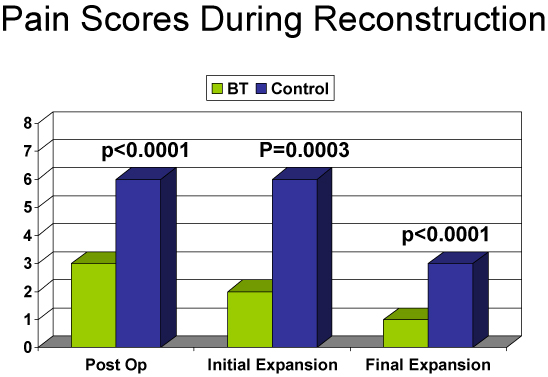
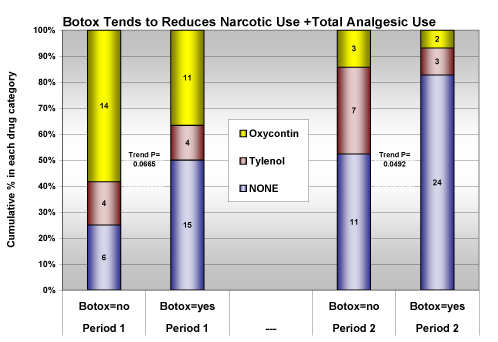
| Objective: To investigate if the intramuscular infiltration of the chest wall musculature with BT after mastectomy with tissue expander placement (M/TE) would inhibit postoperative spasm and pain during expansion. Methods: A prospective non-randomized study was conducted between July 2001 and February 2004. All patients underwent M/TE with (cases) or without (controls) infiltration of 100 units of BT diluted in 40 - 60 cc of normal saline into Pectoralis Major, Serratus Anterior and insertion of Rectus Abdominis. Comparisons were made of procedure indications, demographics and pain, postoperatively and during expansion. Pain was scored using a visual analogue scale of 0-10 (0 = no pain, 10 = worst pain). Wilcoxon rank sum test and the chi-square test were used to test for significance. Results: Fifty-six patients underwent M/TE followed by implant placement; 30(53.5%) with and 26 (46.4%) without BT. The two groups were comparable in terms of age (53+7 yrs vs. 50+3 yrs; p=0.48), bilaterality of procedure (60% vs. 62%; p=0.90), tumor size (1.1+0.2 cm vs. 1.0+0.5 cm; p=0.4), expander size (550+100 cc vs. 450+100 cc; p= 0.23), expansion volume (445+95 cc vs.; 450+70 cc p=0.67) and percentage expansion achieved (78+12% vs. 90+17%; p= 0.18). The BT group did significantly better in terms of postoperative pain (score of 3+1 vs. 6+1; p<0.0001), morphine used during 24 hours postoperatively (2+1 mg vs. 19+9 mg; p=0.0003), pain during initial expansion (score of 2+1 vs. 6+2; p< 0.0001), pain during final expansion (0+1 vs. 3+2; p=0.003) and number of sessions required to achieve target expansion (4+1 vs. 7+3; p=0.025). One patient required a repeat BT infiltration under ultrasound guidance. There was significant difference in length of hospital stay between BT group and controls (23+7 vs. 37+12 hours; p=0.01); however time to permanent implant placement was not significantly different (6+3 vs. 7+4 months; p= 0.44). One expander (due to pain) in the BT group and 5 (2 due to infection and 3 due to pain) in the control group were removed before plan (p=0.13). No complications related to BT injections were reported. Conclusion: Muscular infiltration of BT for M/TE significantly reduced postoperative pain and discomfort due to tissue expansion without complications. |