Sunday, October 28, 2007
12747
Autologous Breast Reconstruction: The Vanderbilt Experience 1998-2005, Independent Predictors of Displeasing Outcomes
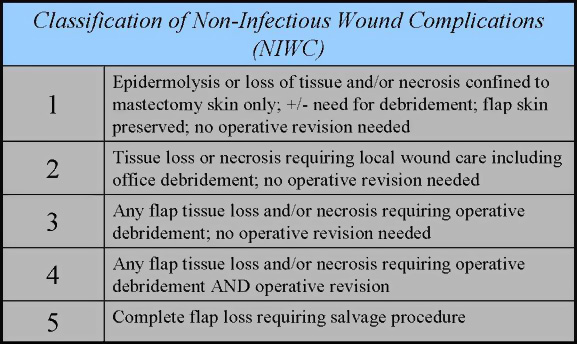
Purpose: In today's society, more patients than ever before seek reconstruction following breast cancer resection that provides aesthetically acceptable results with minimal risk for unfavorable outcomes. Optimized surgical planning and informed consent is dependent on an appreciation for co-morbid conditions that may handicap the reconstructive result. Therefore, the purpose of this institutional review is to delineate independent risk factors for complications following autologous breast reconstruction. Methods: An institutional database was constructed via electronic medical record for all patients who underwent autologous breast reconstruction from 1998 through 2005. Demographic variables captured included: patient age, diabetic and smoking status, pre-reconstruction radiation therapy (XRT), concomitant breast resection, pre-operative albumin level, and the type of reconstruction (Latissimus Dorsi (LD) versus TRAM). BMI was treated as a continuous variable and also categorized based on WHO classifications (BMI >25 = overweight, >30 = obese). The primary outcome was presence or absence of a non-infectious wound complication (NIWC), which is a novel classification of wound problems based on the extent of tissue derangement and the need for escalating surgical correction (see table image). Secondary outcomes were infection, hematoma, hernia (for TRAMs), and fat necrosis. A Cox regression model was tested with the preceding variables serving as controlled co-variates. Results: The analysis included 200 flaps in 180 patients (171 TRAM & 29 LD). Of the TRAMs, 87% were unipedicled, 7% bipedicled, 5% free, & 1% delayed. LDs were almost entirely performed with either tissue expanders or implants. Of the 200 total flaps, there were 19 infections (9.5%), 3 total flap losses (1.5%), 14 hematomas (7%), and 11 donor-site hernias (6%). The incidence of fat necrosis and any NIWC was 18% and 36% respectively. Mean follow-up interval for all patients was 13.1 months (range 1.1-51.7 months). Cox regression demonstrates that BMI > 30 is a statistically significant independent risk factor for any NIWC (HR = 6.58; 95% CI 2.85 ¨C 15.18; p < 0.01) and for NIWC requiring operative treatment (NIWC °Ý 3) (HR = 6.23; 95%CI 2.15 ¨C 18.05; p < 0.01). When treated as a continuous variable in the regression model, BMI is a significant risk factor for NIWC (p <0.01), NIWC requiring operative intervention (p < 0.01), and for culture positive infection (p < 0.01). No other variable including age, diabetes, or smoking served as an independent indicator for any undesirable outcome in this regression model. Conclusions: These data suggest that BMI is a strong predictor of non-infectious wound complications both simple and complex, and of infection following autologous breast reconstruction after adjusting for all other variables in the model. Patients who are obese should be counseled regarding their significantly increased risk of experiencing these unwanted complications.
View Synopsis (.doc format, 113.0 kb)