Sunday, October 28, 2007
13127
Anatomy and Clinical Study of the Postauricular Fascia in Rhinoplasty
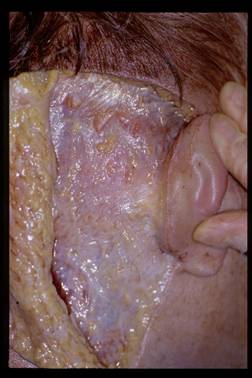
In a previous publication the anatomy and variations of the postauricular muscle complex (PMC) was analyzed and documented. In all dissections, the PMC was covered by a formidable fascial structure. This paper describes the nature and quality of PMC fascia. Additionally, the clinical application of PMC fascia is demonstrated in 18 rhinoplasty procedures performed over 24 months. In 40 fresh cadaver dissections the muscular and fascial components of the PMC were dissected, analyzed, and photographed. The PMC fascia receives contributions from the occipitalis, trapezius, temporal, sternocleidomastoid, superior auricular, posterior auricular and platysma muscles. In fact, all these muscles are covered by strong fascia made up from these contributions. Consistent findings in all dissections included increasingly thicker fascia as the dissection approached the ear. The thickest fascia was always found immediately behind the auricle and thinned out as the dissection was carried posteriorly, superiorly and inferiorly. The thinnest area of fascia was consistently found over the superior belly of the sternocleidomastoid muscle. A second area of weakness was found over the occipitalis muscle. PMC fascia was found in a large donor area, as much as 10 by 10 centimeters, was always present, strong and pliable.
PMC fascia was utilized in augmentation of the radix and dorsum in the clinical portion of this paper. In the follow up period, PMC fascia demonstrated excellent reliability as a free graft in augmentation of these areas. The results of the augmentation were evaluated quantitatively and qualitatively. Average follow-up time is 14 months. PMC fascia is similar to other fascial donor sites located in the head and neck and has been previously described as a potential donor site for rhinoplasty. Advantages of PMC fascia as a donor include ease of harvest, pliability and a potentially large donor site in a nearby area to the nose. PMC fascia can be easily accessed using a single postauricular sulcus incision that also offers the opportunity to harvest auricular cartilage grafts simultaneously. The anatomic dissection demonstrated that PMC fascia offers pliable tissue with various thicknesses and this allows the surgeon to have more choices when planning augmentation of the nose.
Other advantages of fascia eluded to previously include the pliability and softness of the grafts and the lack of visible edges sometimes encountered with cartilage grafts or biomaterials such as expanded polytetrafluoroethylene. PMC fascia is easier to manipulate and does not require extensive experience with cartilage to reduce the risk of visibility. All grafts are held in place using 4-0 chromic sutures that exit the radix skin. Sutures are held in place using a Steri-Strip and then are cut flush with the skin 1 week after surgery. PMC fascia radix grafts are placed to achieve a 25% overcorrection at the time of surgery. This overcorrection can be distressing to some patients and requires reassurance from the surgeon. In most cases, by 6 to 8 weeks the overcorrection had improved and the contour became stabilized. At an average follow-up of 14 months, PMC fascia grafts continue to be stable. Complications included 2 fluid collections and 2 pain control issues at the donor site and 1 overcorrection at the radix. The patient required a single cortisone injection at 8 weeks to reduce overcorrection at the radix. This stabilized and after 10 months of follow up continues to look well.
The authors find PMC fascia to be a reliable graft in nasal surgery. The donor site is plentiful, produces a pliable graft that is easier to handle than radix cartilage grafts. Placement of the graft does not require the same level of expertise involved with cartilage to avoid visibility and contour irregularities. This is an advantage in clinical rhinoplasty surgery, especially for less experienced with cartilage techniques. Overall, donor and recipient site morbidity rates are low and the early results have been gratifying.
View Synopsis (.doc format, 3176.0 kb)