Sunday, October 28, 2007
13211
Exploring the Effects of Referring General Surgeon's Views on Breast Reconstruction Utilization
Background: Breast reconstruction rates remain low at near 5-15% of patients despite the safety and high patient satisfaction of these procedures. Reasons for this are multifactorial including the attitudes and biases of the referring breast surgeon, as well as patient factors. In this study, our purpose was to explore the attitudes of breast surgeons towards breast reconstruction.
Methods: We surveyed 369 General Surgeons in Wisconsin with questions about breast surgery and ideas and opinions about breast reconstruction. We received responses from 36% of surgeons surveyed.
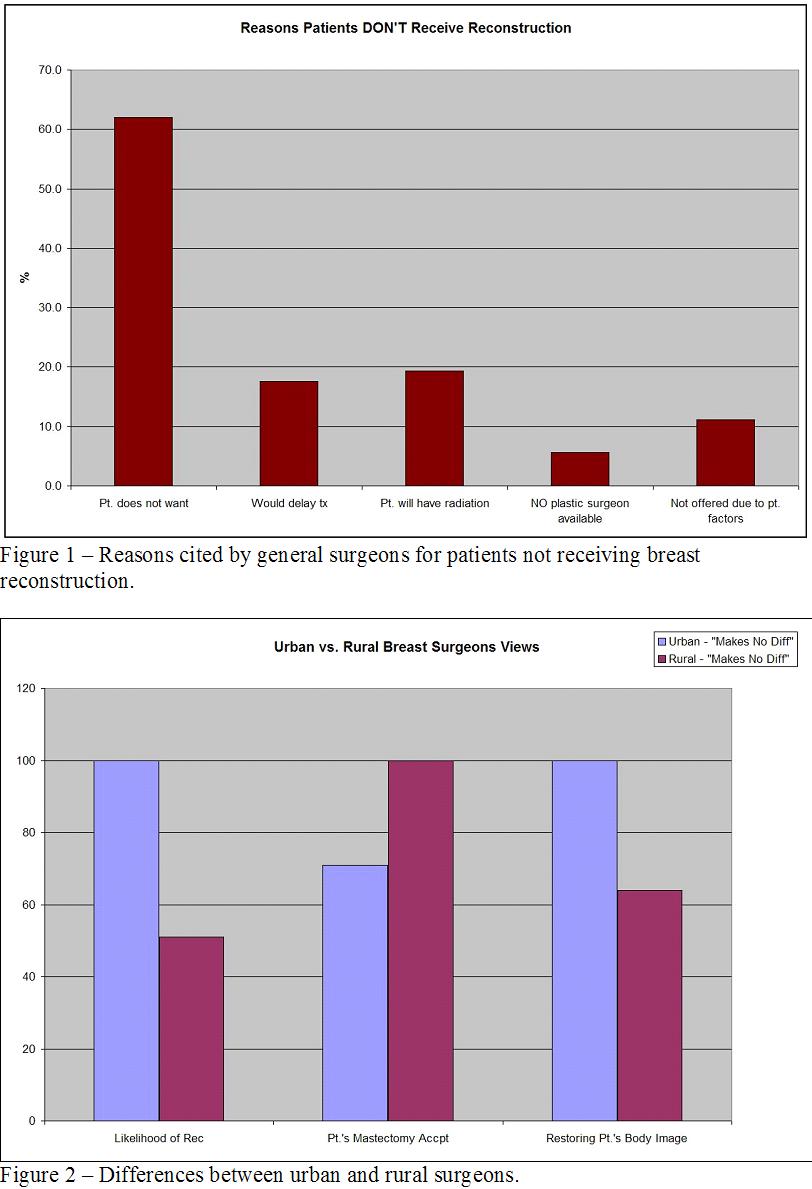
Results: 73% of the respondents performed at least some breast surgery and were eligible for the study. For a little over 50% of the general surgeons surveyed, breast surgery made up less than 10% of their practice. Most (88%) of the respondents never performed nipple sparing mastectomies and 51% never performed a skin-sparing mastectomy. A small number of general surgeons also report performing onco-plastic breast procedures (10%). We found that a large number of breast surgeons (40%) do not routinely refer all mastectomy patients for reconstruction. Reasons that breast surgeons cited as having for not referring patients for reconstruction include the likelihood of cancer recurrence, patient co-morbidities, and high care-taker burden. Patient marital status, household income, and patient education had no effect on referral to a plastic surgeon. Reasons reported by respondents for patients not getting reconstruction included patient's refusal, need for radiation therapy, delaying adjuvant oncologic treatment, patient factors, and having no plastic surgeon available locally (Fig. 1). Respondents generally felt that there was no one type of breast reconstruction that was aesthetically superior (Tissue expander, TRAM, Latissimus dorsi with implant, free TRAM, free DIEP). Surprisingly, 48% of general surgeons believe that tissue expansion reconstruction has the fewest complications. On subgroup analysis, community-based surgeons believed that TRAM flaps give superior aesthetic results. Additionally, 45% of community-based surgeons considered age to be a factor in referral for breast reconstruction. Community-based surgeons cited difficulty in coordinating a two-person team (30%) and having no plastic surgeons available (20%) as reasons for referring patients post-mastectomy. The differences in responses between breast surgeons from urban and rural counties were also examined (Fig. 2).
Conclusions: The decision by a patient to undergo breast reconstruction involves many complex factors. As a specialty, we should focus on improving the availability of breast reconstructive surgeons and educating referring surgeons and patients about reconstructive indications and options in order to positively affect the utilization of breast reconstruction.
View Synopsis (.doc format, 2555.0 kb)