Sunday, October 28, 2007
13357
Biomechanical and Histological Evaluation of Norian CRS and Norian CRS Fast Set Putty in the Long-term Reconstruction of Full-thickness Skull Defects in a Sheep Model
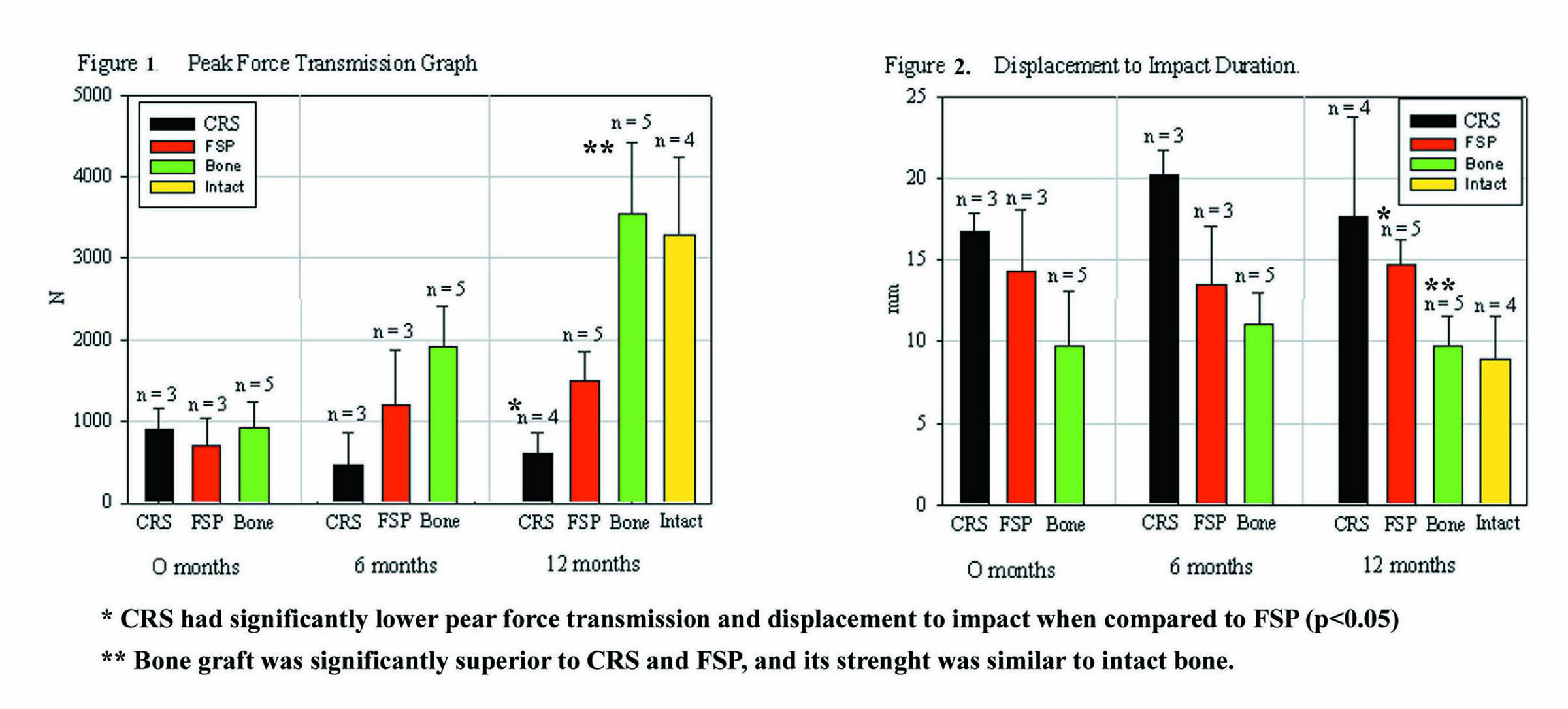
Purpose: To investigate the long-term (12 month) strength and osteoconductive properties of two forms of carbonated calcium phosphate cements (Norian Cranial Reconstruction System [CRS] and Norian CRS Fast Set Putty [FSP]) and to compare these two bone cement forms to an autogenous cranial bone graft in a full-thickness skull defect adult sheep model. Method: This is an experimental animal study in which 26 sheep were assigned to one of eight groups (n=3/group). A 4.5cm2 full-thickness defect was created in the right and left parietal bones respectively. Reconstruction was performed with a full-thickness cranial bone autograft, CRS, or FSP (Figure 1). For bone cement reconstructions of the full-thickness skull defects a titanium mesh was molded to ft the defect contour and then fixed using micro screws to the surrounding superficial surface of the native bone. Wound closure was performed once the material was completely dry (20 min for CRS and 5 min for FSP, at 370C.) Skull samples were harvested at day 1, 6 months and 12 months. Histologic samples were embedded in Spur's Plastic and stained with hematoxylin & eosin (H&E). Biomechanical testing was performed using a vertical drop test, as established by the American Society of Testing and Materials (ASTM). For statistical analysis the peak force transmission (N) - energy absorption of the reconstruction during fracture, the peak acceleration (g) - maximum negative acceleration of the impacting anvil which yields the force required to fracture the cranial reconstruction, the displacement at the impact region of the skull and time to peak acceleration (mm) were recorded. One factor ANOVA (p<0.05) was used to analyze the strength of each reconstruction. Results: Bone grafts were completely incorporated. Although CRS and FSP fully osseointegrated, there was little osteoconduction into the center of these bone cement implants at 12 months. At time zero, there were no significant differences in peak acceleration (p=0.1577) or peak force transmission (p=0.6105) between bone graft, CRS and Fast Set Putty. At one year, significant differences were observed among the three groups. The first generation CRS had the lowest peak acceleration when compared to the Fast Set Putty and bone graft (p< 0.0001) (Figure 1). CRS also showed a decrease in peak force transmission over time, being the weakest of the three reconstructions. The FSP demonstrated a statistically significant increase in both peak acceleration and peak force transmission at 6 months. At one year, FSP was significantly stronger than the CRS (p=0.005), but not as strong as the autogenous cranial bone graft or intact bone (approximately 100% strength) (Figure 2). Cranial bone grafts behaved similar to intact bone and were significantly stronger than CRS and FSP (p<0.0001). At one year, both CRS and FSP cements demonstrated excellent osteointegration and extensive bone apposition with no sign of inflammatory reaction on either the dural or periosteal surfaces. New bone formation could be observed at the bone-cement interface, on the dural and on the periosteal surfaces of the cements. Only a small proportion of the overall volume of cement was resorbed and replaced with bone during the study period. There was almost no osteoconduction into the center of the constructs and osteoconduction appeared to occur only along fracture lines in the cement. Conclusion: CRS progressively lost strength over the course of this study. FSP demonstrated greater strength and rigidity then CRS. Both implants had limited bone ingrowth from defect borders but both cements completely osteointegrated. Bone grafts regained biostructural characteristics and strength similar to intact bone and clinically performed the same in this sheep model.