Tuesday, October 30, 2007 - 8:20 AM
13443
A Financial Analysis of Operative Facial Fracture Management
Purpose: Although essential to the academic mission of any plastic surgery training program, trauma care is associated with low reimbursement rates, placing an economic burden on hospitals and physicians (1, 2). However, the economic impact of operative facial fracture management has not been systematically investigated. This study aims to provide a descriptive financial analysis of all patients undergoing operative facial fracture management at a single academic medical center during a three year period.
Methods and Materials: The records of 202 patients who underwent operative facial fracture management at a United States level one trauma center between 2003 and 2005 were analyzed retrospectively. Demographic, clinical, and financial data were reviewed. All physician and hospital charges related to fracture management, including staged (secondary) operations performed between the time of trauma and the end of 2006, were included. Physician (professional) charges were subdivided by specialty. Total hospital charges (including emergency room, operating room, recovery room, intensive care unit stay, hospital bed, supply charges, pharmaceuticals, laboratory charges, and radiographs) were calculated. Physician reimbursement rates are reported for each specialty and by payer type. To serve as a crude basis for comparison, professional charges and collections for patients undergoing operative facial fracture management were compared to those for the population of general plastic surgery patients and for the population of orthopedic trauma patients over the same time period.
Results: The average patient age was 33.2 years ± 14.6 (std dev); the age range was 3-79 years. Of 202 patients, 146 were male (72%), and 56 were female (28%). The sum of all professional charges billed to these 202 patients was $2,478,234.20 (average of $12,268.49 per patient).
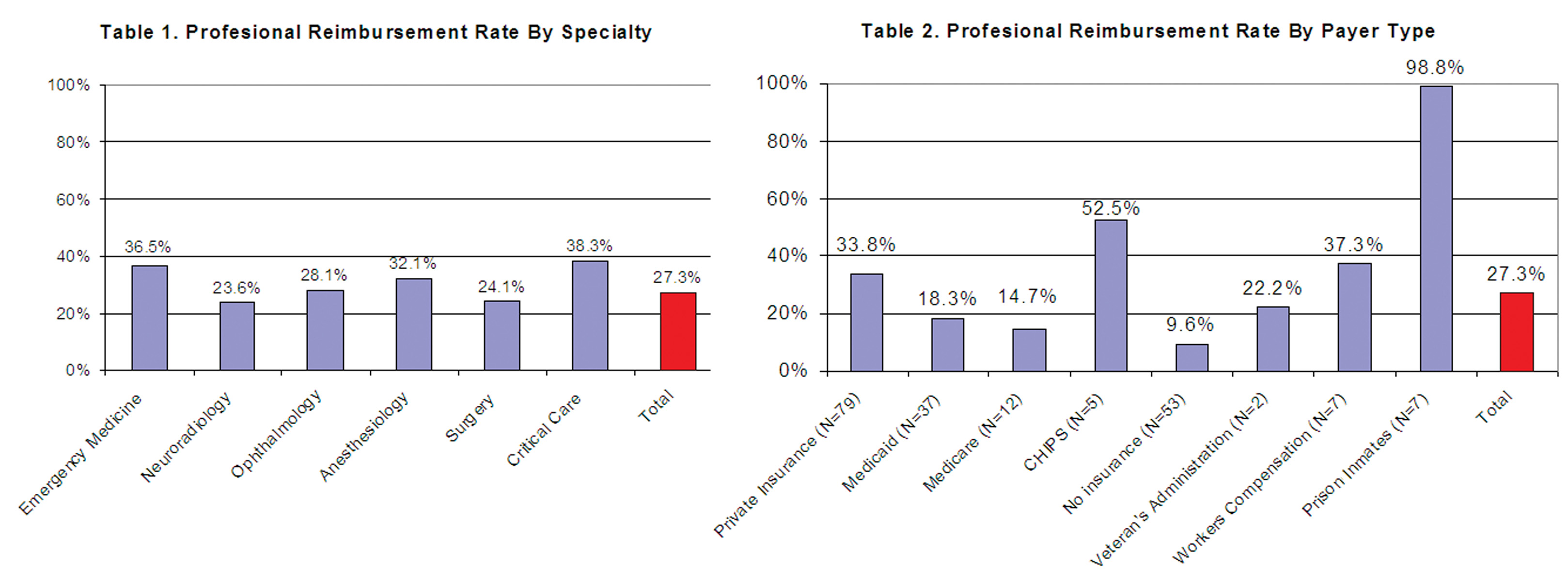
The collections for these professional services totaled $675,434.13, yielding an overall reimbursement rate of 27%. Reimbursement rates ranged from 38% for critical care (ICU) physicians to a low of 24% for surgeons and neuroradiologists. Reimbursement rates are shown in figure 1 for each physician specialty type.
When analyzed by payer type, the highest reimbursement rates were seen in children covered by CHIPS and in federal and state prison inmates (53% and 99% respectively). The lowest reimbursement rate was obtained from uninsured patients (26% of patients), who paid an average of 10% of physician charges. Professional reimbursement rates for each payer type are shown in table 2. Private insurance reimbursed at slightly higher than the average rate.
The total hospital charges for the same patient group was $18,120,027 (average of $89,703.10 per patient); total collections were $2,770,115 (15% reimbursement rate).
For comparison, the total professional charges for operative management of orthopedic skeletal trauma over the study period was $173,702,951, with total collections of $57,223,826, which equals a 33% reimbursement rate. The total billings for professional services within the Division of Plastic Surgery during the same period was $32,559,264 of which $10,352,944 was collected (reimbursement rate 32%).
Conclusions: This study provides an up-to-date economic analysis of operative facial fracture management at a major United States trauma center. Within the limits of a simple descriptive analysis of charges and collections, our results appear to demonstrate the unfavorable financial circumstances associated with facial trauma care. From a purely financial standpoint, these economic realities make facial trauma relatively unrewarding, and present a challenge to academic plastic surgery.
References: 1. Shapiro MJ, Keegan M, Copeland J. The misconception of trauma reimbursement. Arch Surg 1989; 124(10):1237-40. 2. Henry MC, Thode HC, Jr., Shrestha C, Noack P. Inadequate hospital reimbursement for victims of motor vehicle crashes due to health reform legislation. Ann Emerg Med 2000; 35(3):277-82.
Figure Legend: Figure 1. Professional reimbursement rates for 202 patients undergoing operative management of facial fractures for each physician specialty category. Figure 2. Professional reimbursement rates for each payer type.
View Synopsis (.doc format, 777.0 kb)
See more of Cranio/Maxillofacial/Head & Neck
Back to 2007am Complete Scientific Program