Sunday, October 28, 2007
13521
Management of Neonatal Upper Airway Obstruction: Decreased Morbidity by Utilizing a Decision Tree Model with Mandibular Distraction Osteogenesis
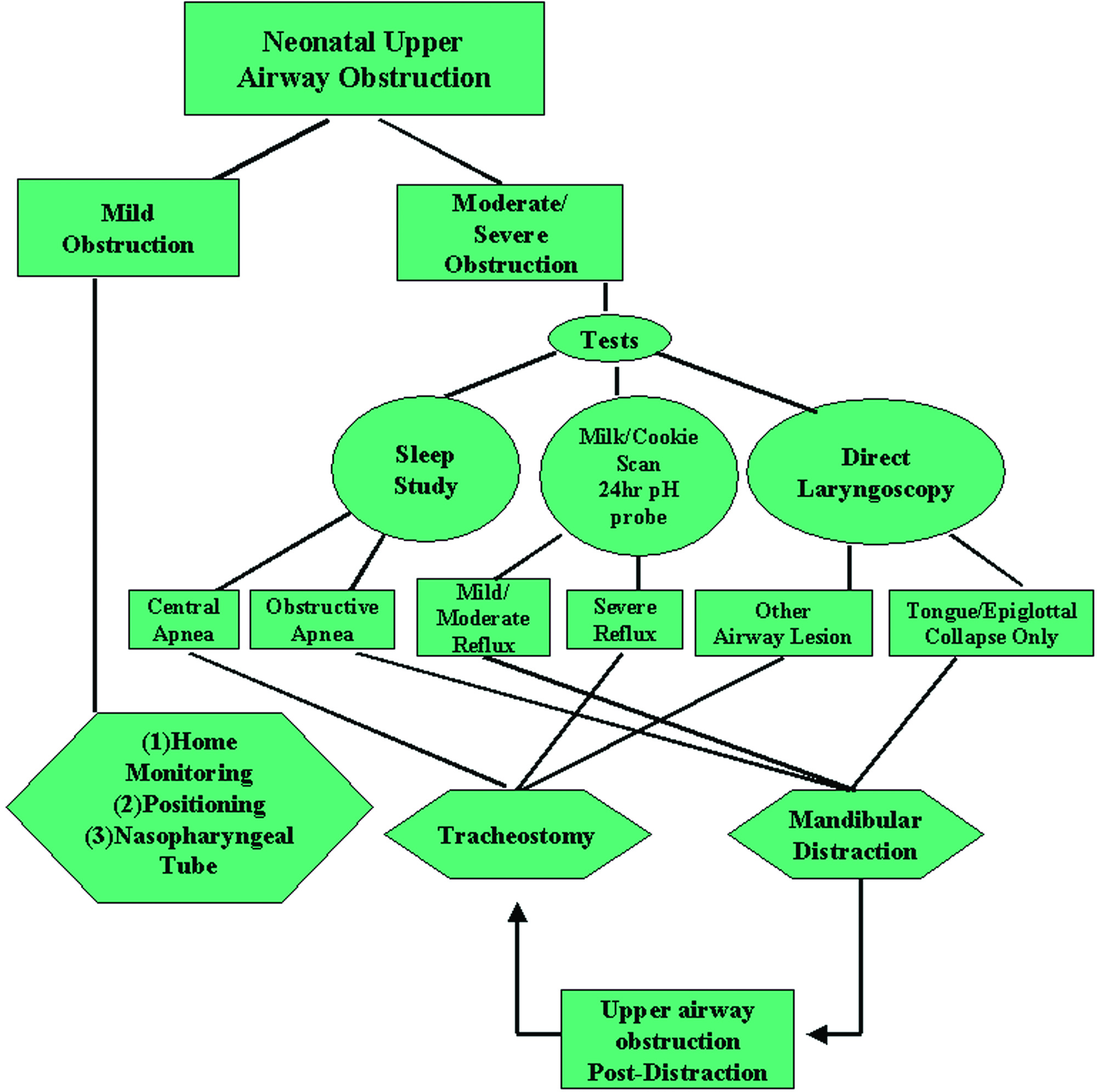
Background/ Purpose: For craniofacial syndromic patients, neonatal upper airway obstruction requires urgent management. While tracheostomy may be life-saving in these circumstances, it is associated with numerous morbidities, long-term speech and growth delay. Distraction osteogenesis or mandibular jaw lengthening offers an alternative to tracheostomy, but proper patient selection requires the plastic surgeon obtain appropriate studies and make timely decisions.
Methods: A ten-year review of neonates with upper airway obstruction at two academic centers was performed (n=149). We compared conventionally treated neonates (control group), receiving home monitoring or a tracheostomy on a case by case basis, to newborns managed by a new decision tree model (DTM) (study group), in which a specific pattern of diagnostic tests and specialist consultations were obtained to decide among home monitoring, tracheostomy, or distraction. Long-term outcomes in mortality, morbidity, speech, and growth were assessed.
Results: Neonates managed with our DTM were significantly less likely to undergo a tracheostomy than those managed conventionally (28% versus 82%, p<0.05). No deaths occurred and only one of 43 children in our DTM group who initially underwent DO required subsequent tracheostomy (for unrecognized central apnea). There were three deaths in conventionally managed neonates compared to none in the study group. All three deaths in the control group were airway-related, including two deaths in patients managed with home positional monitoring. Newborns managed with our DTM had significantly fewer hospital days (mean 18 vs. 33, p<0.05), emergency department visits (3.4 vs. 9.6, p<0.05), pneumonia (4% vs. 24%, p<0.05), gastrointestinal reflux (12% vs. 69%), and feeding problems (9% vs. 61%, p<0.05) compared to their conventionally treated counterparts. Study group patients showed improved height (60th percentile) and weight (64th percentile) compared to control group subjects (42nd and 28th percentile, respectively, p < 0.05). With regard to lower facial profile measured by lateral profilogram, there was a statistically significant increase in lower facial profile in those children managed with the DTM compared to those managed conventionally (23% versus 5%, p < 0.05). Sixty children in the study group (78%) and 22 in the control group (31%) were tracheostomy free at final follow-up and had some degree of speech (chi-square, p < 0.05). Of these, there was no significant difference in incidence of VPI between the study and control groups (16% versus 18%). Patients with a remaining tracheostomy demonstrated minimal to no understandable speech and communicated primarily with sign language or hand signals at final follow-up.
Conclusions: In treating newborns with micrognathia and upper airway obstruction, a plastic surgeon will have better patient outcomes when utilizing a decision tree model with multidisciplinary specialists, timely studies, and an option for mandibular distraction osteogenesis.